Cardiovascular
Associations of shift work and eating duration with cardiometabolic health and biological age acceleration among U.S. workers Xuyuehe Ren* Xuyuehe Ren Liwei Chen Jian Li
Objectives: Shift work schedules and eating duration can both influence circadian rhythm, which is crucial for cardiometabolic health and longevity. We aimed to examine the independent and joint associations of shift work (SW) and short eating duration (SED) with cardiometabolic diseases (CMD) and biological age acceleration (BAA) in a nationally representative sample of U.S. workers.
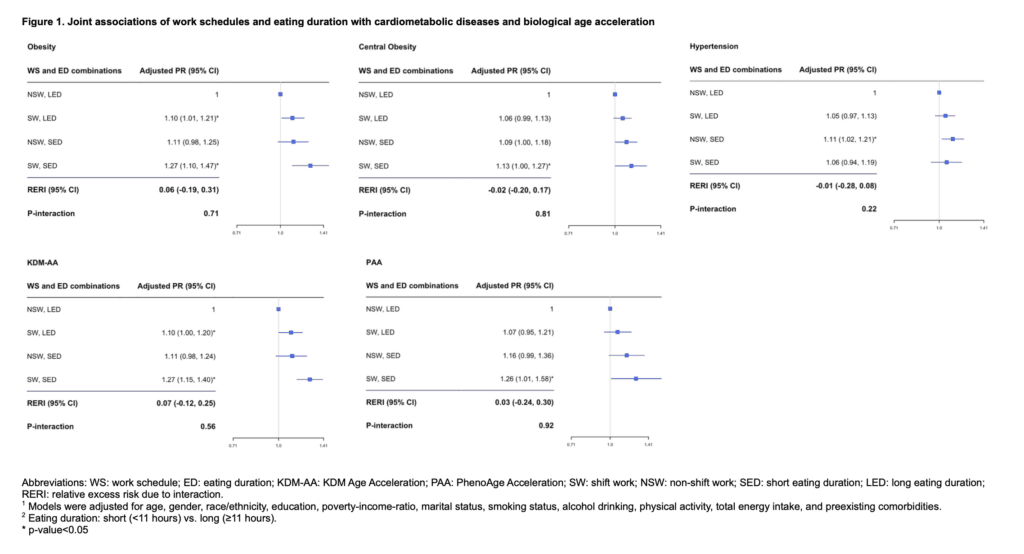
Methods: We included 30,299 eligible workers from the National Health and Nutrition Examination Survey 1999-2020. Work schedules were self-reported and classified as SW vs. non-shift work (NSW). Time of eating occasions were accessed by 24-hour dietary recalls, and eating duration was classified as SED (<11h) vs. long eating duration (LED: ≥11h) based on exploratory analyses for threshold effects. CMD were ascertained by self-reported physician diagnosis, medication use, or clinical markers. BAA was calculated as the difference between biological age (estimated using Klemera and Doubal method (KDM-AA) and PhenoAge algorithms (PAA)) and chronological age, then dichotomized at zero. Adjusted Poisson regressions were used to cross-sectionally examine the independent and joint associations of SW and SED with the prevalence of obesity, central obesity, hypertension, and BAA.
Results: SW was associated with higher prevalences of obesity (PR, 1.22; 95%CI, 1.10-1.35), central obesity (PR, 1.18; 95%CI, 1.03-1.34), and positive BAA (KDM-AA: PR, 1.14, 95%CI, 1.08-1.21; PAA: PR, 1.12, 95%CI, 1.04-1.19). Similarly, SED was associated with higher prevalences of obesity (PR, 1.11; 95%CI, 1.10-1.35), central obesity (PR, 1.09; 95%CI, 1.04-1.14), and positive BAA (KDM-AA: PR, 1.13, 95%CI, 1.07-1.21; PAA: PR, 1.19, 95%CI, 1.08-1.33). There was suggestive evidence that workers exposed to both SW and SED had higher prevalences of obesity, central obesity, and positive BAA than those with NSW and LED.
Conclusions: Workers with SW, SED, or both were more likely to have obesity, central obesity, and BAA.