Environment/Climate Change
Examining Interaction on an Additive Scale between Short-Term Ambient Air Pollution Exposure and Cardiovascular Disease for Risk of Adverse COVID-19 Outcomes Sneha Kannoth* Sneha Kannoth Pam Factor-Litvak Stephen S. Morse Earle C. Chambers Kristen M. Rappazzo Cong Zhang Sandra S. Albrecht Alexander Azan Min Qian Perry E. Sheffield Azure Thompson Jennifer A. Woo Baidal Stephanie Lovinsky-Desir Jeanette A. Stingone
Introduction
Research suggests a link between short-term particulate matter (PM2.5) exposure and adverse COVID-19 outcomes. Cardiovascular disease (CVD), a COVID-19 risk factor, may increase vulnerability to the effects of short-term PM2.5. We assessed whether short-term PM2.5 and CVD interact to induce greater risk of adverse COVID-19 outcomes.
Methods
We used NYC COVID-19 hospitalization records (Mar-Dec 2020; N=15361). Short-term PM2.5 was a 7-day residential ZIP Code average before hospital admission, using EPA Community Multi-Scale Air Quality modeled data. CVD was defined using 15 common cardiovascular conditions, such as atrial fibrillation, cerebrovascular disease, myocardial infarction, etc. We estimated the relative excess risk of interaction (RERI) between short-term PM2.5 and CVD on adverse COVID-19. We used targeted maximum likelihood estimation (TMLE) to assess the average treatment effect (ATE) of short-term PM2.5 on adverse COVID-19, among those with and without CVD. Modified Poisson regression estimated the risk of acute respiratory distress syndrome, pneumonia, ventilation, and dialysis and Cox regression estimated the risk of fatality and discharge, adjusting for age, sex, smoking, and environmental vulnerability.
Results
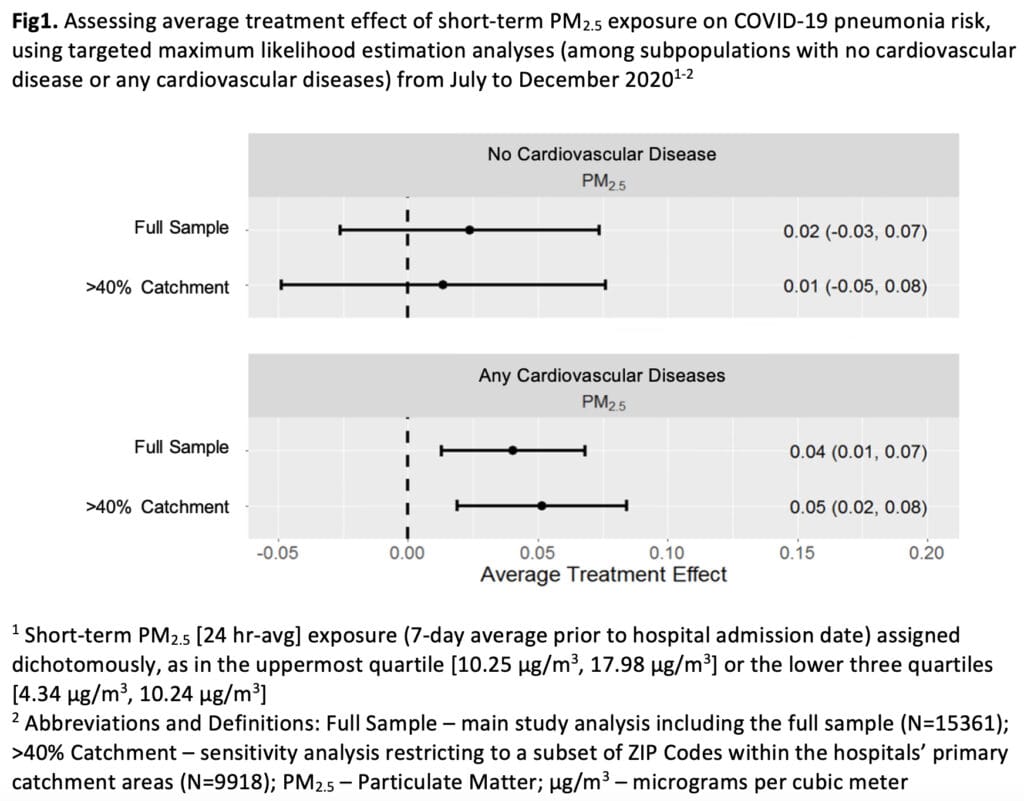
We observed synergistic interaction between short-term PM2.5 and CVD for pneumonia risk from July to Dec 2020 (e.g., myocardial infarction (RERI:0.30; 95%CI:0.05-0.55), atrial fibrillation (RERI:0.23; 95%CI:0.05-0.40)). TMLE analyses suggest that short-term PM2.5 increased risk of pneumonia only among those with CVD (ATE:0.04, 95%CI:0.01-0.07; Fig1).
Discussion
Short-term PM2.5 interacts with CVD to induce greater risk of COVID-19 pneumonia in the latter half of 2020, which had higher short-term PM2.5 variability. TMLE analyses suggest short-term air pollution reductions targeted towards those with greater health vulnerability (i.e., greater cardiovascular burden) may reduce incidence of acute respiratory infections, such as pneumonia.