LATEBREAKER
COVID-19 Pandemic
A novel method for the classification of medical environment features in COVID-19 research Edwin McCulley* Edwin McCulley Usama Bilal Gina Lovasi Brisa Sanchez Alinan Schnake-Mahl Jana Hirsch
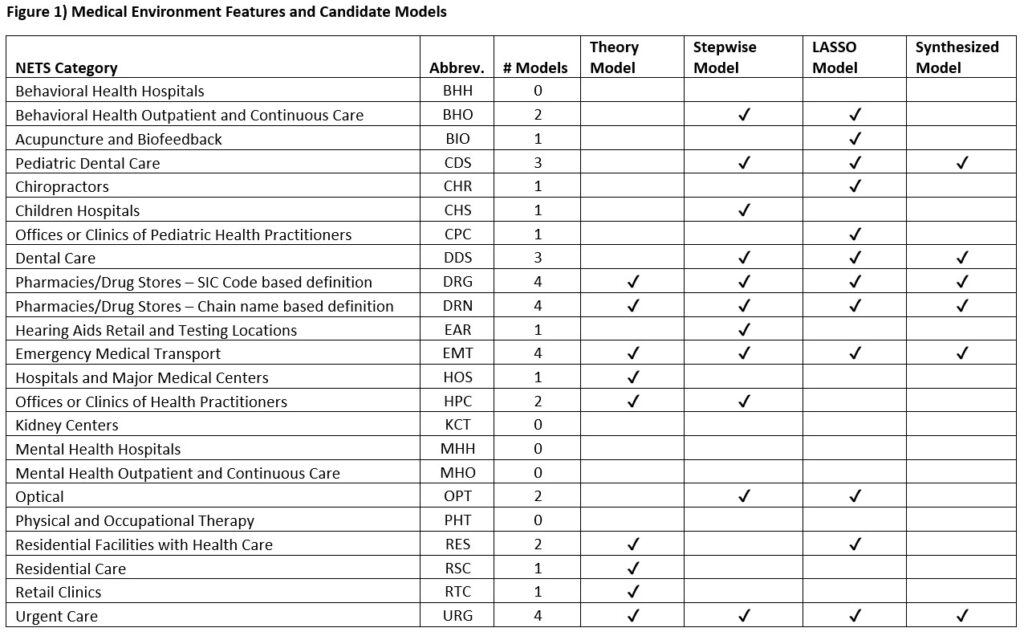
The COVID-19 pandemic disproportionately affected vulnerable populations worldwide. Some faced greater risk of severe COVID-19 outcomes due to individual factors like preexisting medical conditions, while others were affected by environmental factors such as the presence or absence of medical facilities that provide lifesaving care. Despite investigations into the individual factors that predispose individuals to severe COVID-19, less attention has been paid to the contextual effects of place-based environmental factors on COVID-19 outcomes. We aimed to compare 4 methods of measuring COVID-19-relevant features in the nearby medical environment (ME). We utilized individual mortality data on COVID-19 deaths from the National Center for Health Statistics to compute rates of COVID-19 deaths in US counties from 2020-2021. We obtained local ME features from the National Establishment Time Series, grouped into 23 categories. We then used Quasi-Poisson Generalized Linear Models to predict COVID-19 death rates using four approaches: a theory-driven approach based on expert knowledge of three reviewers, a backwards stepwise approach, a Least Absolute Shrinkage and Selection Operator (LASSO) approach, and a synthesized approach which included predictors that were relevant across two or more models. Each model identified several COVID-19-relevant ME features (Figure 1), with the stepwise and LASSO approaches providing the best-fit models based on qAIC. Furthermore, pharmacies/drug stores, emergency medical transport, and urgent care emerged as important predictors of COVID-19 death rates across models, suggesting a critical role in the screening, treatment, and prevention of COVID-19 during year 1 of the pandemic. This novel classification method can help identify ME factors that are predictive of population-level COVID-19 impacts and can guide public health research aimed at reducing or eliminating inequities in COVID-19 outcomes, especially among vulnerable populations.