LATEBREAKER
Health Disparities
Healthcare Discrimination and Adherence to Preventive Services Guidelines in 2023 among a Nationally Representative, Diverse Sample of US Adults Paula Strassle* Paula Strassle Allana T. Forde
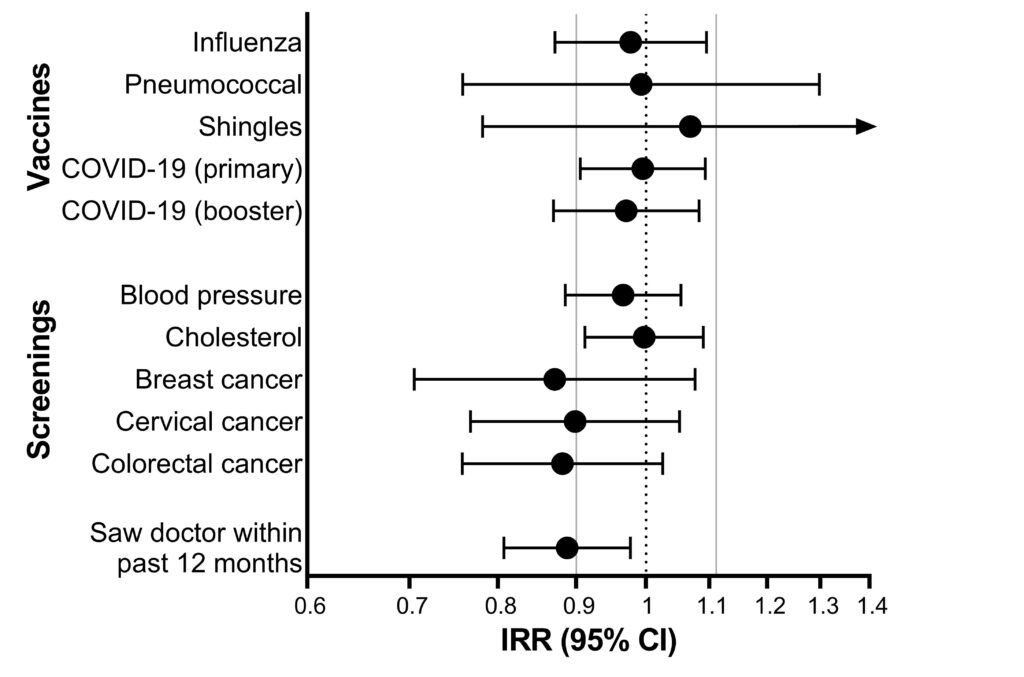
Preventive services, like cancer screenings and vaccinations, represent a critical avenue for reducing disease risk. It remains unclear how barriers, like experiencing healthcare discrimination, impact adherence to preventive services recommendations and potentially exacerbate health disparities. We used data from the Health Equity through Adherence to Preventive Services (HEAPS) study, a nationally representative, online survey of American Indian or Alaska Native (AIAN), Asian, Black/African American (Black/AA), Latino (English and Spanish speaking), Middle Eastern or North African, Native Hawaiian or Pacific Islander, White, and multiracial adults ≥35 years old from 6/2023-8/2023, N=4111. The validated Interpersonal Processes of Care (IPC-18) survey was used to measure discrimination due to race/ethnicity by medical providers. Adherence to preventive services guidelines was measured using a modified Medical Expenditure Panel Survey. Poisson regression with robust variance estimates, adjusting for sociodemographics and insurance status, were used to estimate the association between discrimination and preventive services. Analyses were weighted to be nationally representative within racial and ethnic groups. Overall, 20.0% of participants reported being discriminated by medical providers sometimes/always within the past year; Black/AA participants had the highest prevalence (28.9%), followed by Spanish-speaking Latino (27.4%), and AIAN (23.5%). Adherence to preventive care guidelines ranged from 51.0% to 85.5%. After adjustment, experiencing healthcare discrimination (sometimes/always vs. rarely/never) appeared to reduce breast, cervical, and colorectal cancer screening rates (IRRs 0.87-0.90) but confidence intervals were wide, Fig. Healthcare discrimination was associated with being less likely to have seen a doctor in the past year (IRR=0.89, 95% CI 0.81-0.98). Implementing antidiscrimination strategies could increase healthcare utilization and cancer screenings.