Cardiovascular
Utility of Framingham Stroke Risk Profile for predicting stroke among United States Veterans Serena Houghton* Serena Houghton Timothy Treu Daniel C. Posner Laura Tarko Vasileios-Arsenios Lioutas David R. Gagnon Peter W.F. Wilson Kelly Cho Hugo J. Aparicio
Background: The Framingham Stroke Risk Profile (FSRP) is a validated clinical tool to predict an individual’s risk of stroke and is used in research to assess the incremental utility of novel risk factors. We examined use of the FSRP model among a diverse cohort of US Veterans within the Veterans Health Administration (VHA).
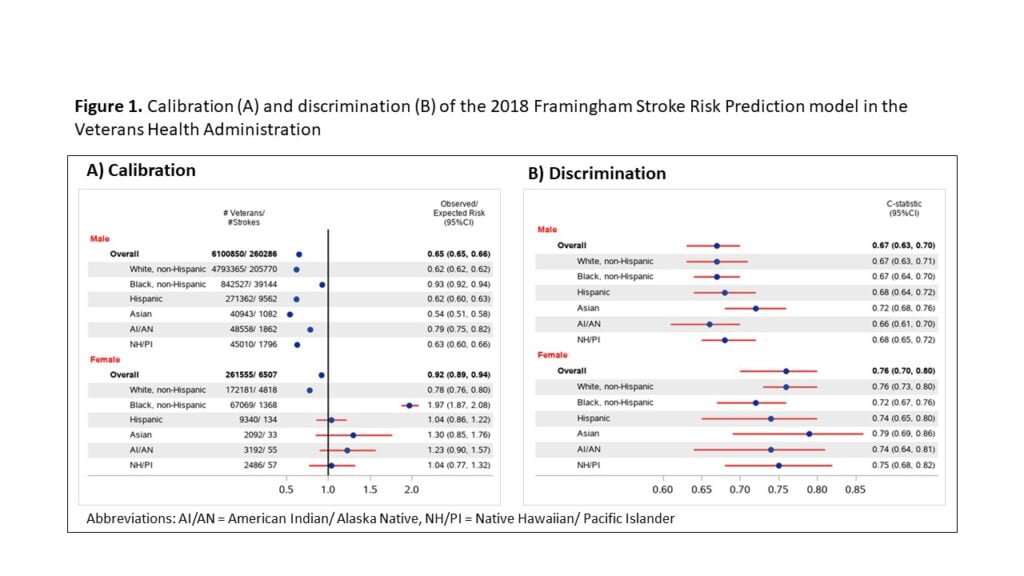
Methods: We included Veterans aged ≥45 years with no prior transient ischemic attack or stroke (N=6,362,405; 96% male) with a primary care visit, blood pressure, and cholesterol measure from 2007-2017 (mean age, y:66.0 [male]; 57.6 [female]). Veterans were followed for stroke up to 10 years (mean:7.3 y) from the blood pressure date, censored at the first of death, last visit date, or end of 2019. Stroke was defined as the first inpatient ICD 9 or 10 diagnosis code (ischemic or hemorrhagic) in the VHA electronic health record, Centers for Medicare and Medicaid Services, or primary cause in the National Death Index for fatal stroke. We examined discrimination (C-statistic [C]) and calibration (Observed/Expected [O/E]) of the FSRP within the VHA for 10-year predicted stroke risk using Cox models stratified by sex and race/ethnicity.
Results: There were 260,286 (4.3%) incident strokes among males and 6,507 (2.5%) among females. The FSRP showed weaker discrimination in males (C:0.67, 95%CI:0.63-0.70) compared to females (C:0.76, 95% CI:0.70-0.80). Discrimination was higher in Asian Veterans compared to other racial/ethnic groups. The FSRP overestimated 10-year stroke risk in Veterans overall (O/E:0.65 male; 0.92 female) and in most race/ethnicity subgroups; however, it underestimated risk in Black women (O:2.8%; E:1.5%).
Conclusion: In a large, diverse cohort of Veterans, the ability to predict stroke using the FSRP varied by sex, race, and ethnicity. Consideration of these factors, as well as recalibration and the addition of Veteran-specific risk factors (e.g., combat history, traumatic brain injury) may improve the model’s predictive ability.