Infectious Disease
Effect of Seasonal Malaria Chemoprevention (SMC) on malaria transmission: Analysis of 2021 malaria rates in Nouna, Burkina Faso Elisabeth Gebreegziabher* Elisabeth Gebreegziabher Mamadou Ouattara Ali Sié Mamadou Bountogo Boubacar Coulibaly Valentin Boudo Thierry Ouedraogo Elodie Lebas Huiyu Hu Benjamin F. Arnold Thomas M. Lietman Catherine E. Oldenburg
Objective
Seasonal malaria chemoprevention (SMC) is the administration of sulfadoxine–pyrimethamine (combination of a broad-spectrum antibiotic, sulfadoxine and antiparasitic pyrimethamine) and amodiaquine to children aged 3-59 months at monthly intervals four times during the high malaria transmission season. Using data from the Community Health with Azithromycin Trial (CHAT), a randomized controlled trial of 278 villages in Nouna Burkina Faso, passive surveillance data of clinic visits and national malaria control program (NMCP) data on SMC administration, this study aimed to describe malaria incidence rates in the presence of SMC and compare malaria rates in the weeks after administration of SMC.
Methods
For each health post in the study area, we calculated the malaria diagnoses counts by epidemiological (epi) week. We used CHAT census data to obtain denominators, number of children by health post, to estimate the malaria rates for each epi week in 2021. Negative binomial regression was used with person weeks used as offset and standard errors clustered by health post to obtain incidence rate ratio (IRR) comparing malaria rates over the four rounds of SMC administration weeks to the first, second-, and third-weeks post administration.
Results
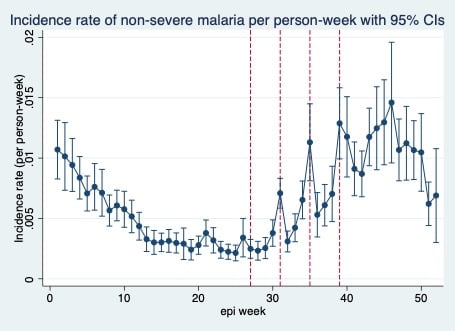
In 2021, SMC was administered in four rounds four weeks apart between July and September, on epi weeks 27, 31, 35 and 39. SMC was administered during malaria peak weeks (Incidence rate (IR)= 8.4, 95% CI (6.8 to 10.1) per 1000 person weeks). Malaria rates were still high through December, after fourth/last round of SMC (IR range 10-15 cases per 1000 person weeks). There was substantial reduction in malaria rates in the 3 weeks post SMC, but not in linear fashion. Compared to administration weeks, malaria rates were lower by 36%, 37% and 23% in the first, second and third week after administration (IRR= 0.64, 95%CI (0.55 to 0.76), 0.63, 95%CI (0.55 to 0.73) and 0.77, 95%CI (0.67 to 0.88) respectively).
Conclusion
Our findings suggest that four rounds of administration may not adequately cover the malaria transmission season. A fifth round of SMC could be helpful. The greatest decline in malaria rates post SMC was in the first two weeks after administration and rates started to increase by week 3. SMC appears effective but short-lived.