HIV / STI
Understanding the relationship between depression and longitudinal HIV care continuum outcomes in a cohort of people entering HIV care in Cameroon Lindsey Filiatreau* Lindsey M. Filiatreau Peter Vanes Ebasone Anastase Dzudie Milton Wainberg Marcel Yotebieng Kathryn Anastos Rogers Ajeh Denis Nash Angela M. Parcesepe
Addressing mental health needs of people with HIV (PWH) has gained mounting traction as a strategy critical to ending the HIV epidemic. Yet, empirical evidence clarifying the relationship between depression and HIV care outcomes across the care continuum is scant. Multi-state methods can provide a holistic picture of how individuals engage and disengage in care over time and aid in understanding complex longitudinal exposure/outcome relationships.
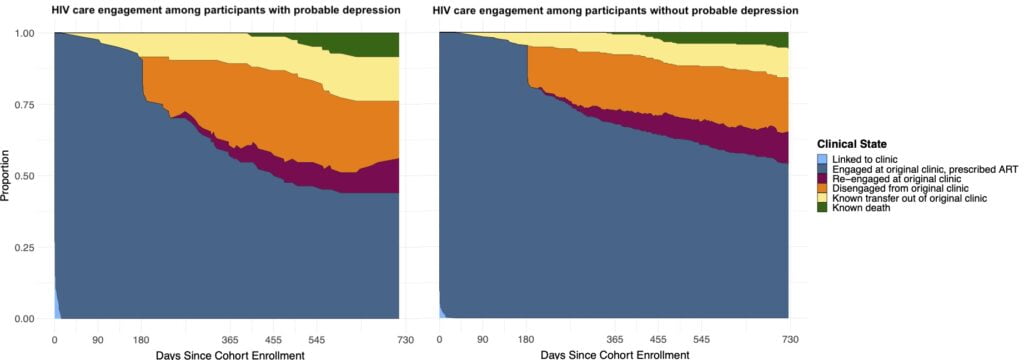
From June 2019-March 2020 we enrolled PWH aged 21+ entering HIV care at 3 clinics in Cameroon. We conducted structured interviews to ascertain demographics and depression status (Patient Health Questionnaire-9 scores>9=probable depression) at enrollment and extracted participant clinical record data through January 1, 2022. We estimated time spent in six mutually exclusive and exhaustive HIV care states: linked to clinic; engaged at clinic, prescribed ART; disengaged from clinic; re-engaged at clinic; known death; known transfer out; and transitions between these states in the first 2 years following enrollment. Estimates were compared for those with vs. without (referent) probable depression using differences.
420 PWH contributed 825.4 person-years of follow-up. 20% (n=81) had probable depression at enrollment. A similar proportion of individuals with and without probable depression failed to return to care after their first visit (~10%). However, those with probable depression were less likely to be engaged in care at both years 1 and 2 [Figure; percent differences of 12.2% and 8.7%, respectively] and consistently demonstrated a higher hazard of transfer out compared to those without probable depression. Of those who disengaged from care, those with probable depression re-engaged later than others (re-engagement hazard peak: days 112 vs. 54).
Routine depression screening and sustained support for PWH with probable depression is warranted for PWH entering HIV care to improve population-level downstream treatment outcomes.