Aging
Descriptive epidemiology of New York City older adult patients with multiple chronic conditions Sarah Conderino* Sarah Conderino John Dodson Yuchen Meng Mark G. Weiner Catherine Rabin Wilson Jacobs Parampreet Bakshi Melissa Lee Jenny Uguru Lorna E. Thorpe
Background: Co-occurrence of multiple chronic conditions (MCCs) is a significant public health concern among older adults, with differential burden by race/ethnicity and sex. Our objective was to characterize comorbidity profiles and cardiometabolic risk factor trajectories among older adults with MCCs in New York City (NYC) using an intersectionality approach.
Methods: Electronic health record (EHR) data were obtained from the INSIGHT Clinical Research Network. The study population included NYC residents aged 50 or older with MCCs with at least one ambulatory visit in the six months before COVID-19 pandemic onset (9/7/2019–3/6/2020). We descriptively characterized comorbidity profiles and assessed the cardiometabolic risk factors of blood pressure, cholesterol, A1C, and weight by the intersection of sex and race/ethnicity.
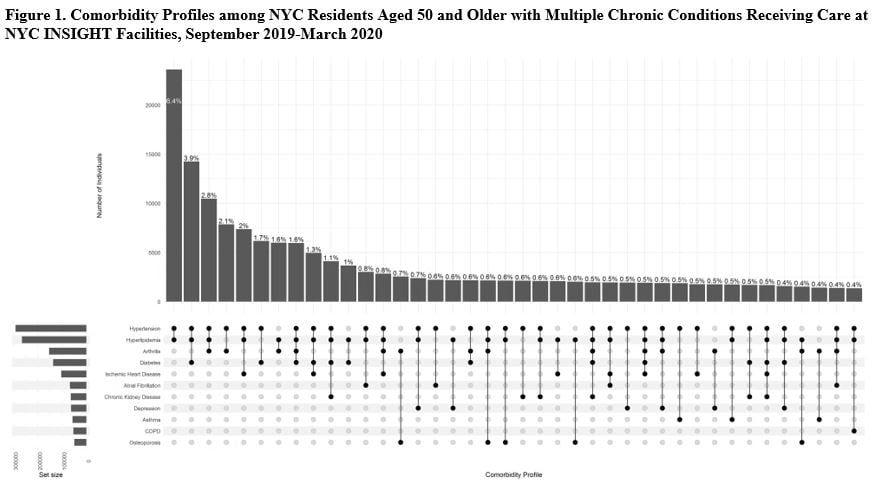
Results: There were 367,901 older adults with MCCs in the INSIGHT sample. Comorbidity profiles were heterogeneous (Figure 1), but the most common profile across sex-and-race/ethnicity groups was co-occurring hypertension and hyperlipidemia (6% alone, 59% in combination with other conditions). Burden of these two conditions differed across groups, with highest hypertension prevalence among Black females (87.3%) and males (87.4%) and highest hyperlipidemia prevalence among Asian (78.9%) and white males (79.0%). Cardiometabolic risk factors also differed significantly, with highest systolic blood pressure among Black females (mean=134.8mmHg) and males (mean=134.8mmHg) and lowest obesity among Asian females (16.5%) and males (15.7%). Across all race/ethnicity groups, females had a higher average LDL cholesterol than males.
Conclusions: Significant disparities were observed in comorbidity burden and cardiometabolic risk factors, which may reflect underlying systems of power and discrimination, such as health care access. Public health interventions are needed to prevent chronic disease onset and improve disease management among minoritized populations.