Health Disparities
Leveraging Disease Misclassification to Estimate the Impact of Pre-Pregnancy Healthcare Access on Maternal Morbidity Ariana Mora* Ariana Mora Michael Kramer Joshua Wallach Mohammed K. Ali Timothy Lash
Background: Undiagnosed pre-pregnancy illness, which can be due to poor healthcare access, likely negatively impacts pregnancy outcomes since the disease is unknown and not medically managed. Increased healthcare utilization during pregnancy may lead to the diagnosis of these previously undiagnosed conditions, but it may also lead to disease misclassification. For example, pre-existing chronic diabetes (DMII) could be misclassified as gestational diabetes (GDM) if first evaluated in the setting of pregnancy. Thus, identifying DMII misclassified as GDM could serve as a proxy for inadequate pre-pregnancy healthcare, which is otherwise unmeasured.
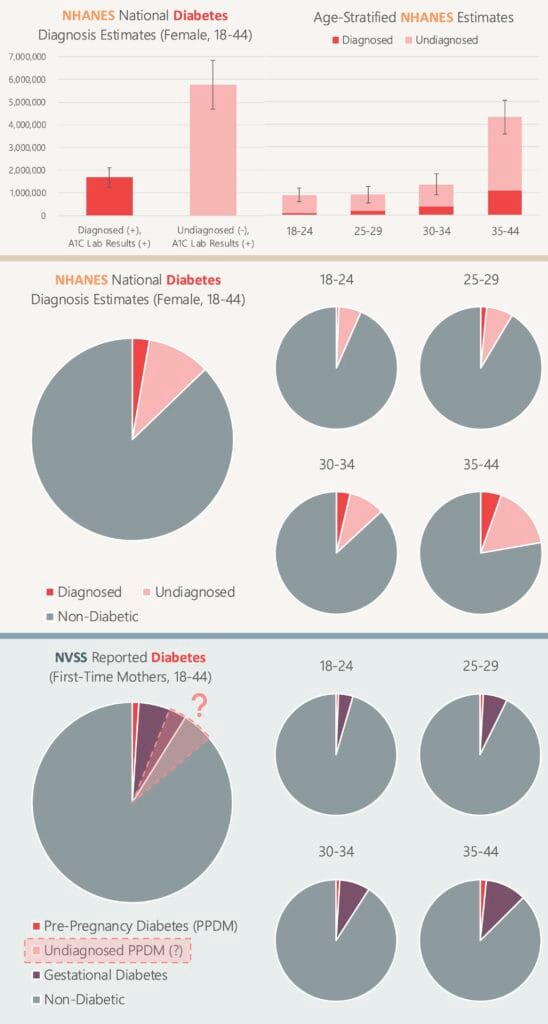
Methods: We used the National Health and Nutrition Examination Survey (NHANES) to compare self-reported DMII diagnosis with clinically validated DMII status and identified individual health and socioeconomic factors predictive of DM misclassification. We then transported individual-level misclassification likelihoods to 2016-2023 natality data in the National Vital Statistics System (NVSS). Bias analysis will compare poor pregnancy outcome risks in reclassified DM births compared to the original NVSS DM classifications.
Results: Among NHANES reproductive age women (18-44), DMII diagnosis has sensitivity 0.24, specificity 0.99, PPV 0.75, and NPV 0.88. Reclassifying NVSS births to adjust for DMII underdiagnosis results in an additional 260,222 births with presumptive DMII (original: 100,713 DMII births). These are preliminary marginal estimates; modeled estimates will account for confounders affecting true underlying DMII and the diagnosis of DMII.
Summary: By leveraging externally informed bias adjustments of surveillance data, this research highlights potential changes to medical screening guidelines to reduce under/misdiagnosis of DM, improve biased estimates for poor pregnancy outcome risk factors, and support policies that increase pre-pregnancy healthcare access to reduce adverse pregnancy outcomes and disparities.