Pharmacoepidemiology
Comparative Effectiveness of Left Atrial Appendage Occlusion versus Oral Anticoagulants in Older Atrial Fibrillation Patients Xiaojuan Liu* Xiaojuan Liu Sebastian Schneeweiss Daniel E. Singer Jerry Avorn Edwin K. Heist Joshua K. Lin
Introduction: Real-world evidence evaluating left atrial appendage occlusion (LAAO) devices vs. oral anticoagulants (OAC) in patients with nonvalvular atrial fibrillation (AF) remain limited. We aimed to compare health outcomes between LAAO device users and OAC users.
Methods: A cohort study including 20992 AF patients aged ≥65 years with a CHA2DS2-VASc score of ≥2 (males) or ≥3 (females), using US Medicare claims data from 2016-2020. Patients who received LAAO in conjunction with OAC (warfarin, apixaban, rivaroxaban, or dabigatran) or with P2Y12 inhibitors on the index date were 1:1 matched to patients who received these medications alone via propensity score matching based on >80 pre-treatment covariates. Outcomes included hospitalization for major bleeding events, ischemic stroke, and all-cause death. Follow-up was censored at 2 years or upon treatment deviation (OAC discontinuation or LAAO implantation in OAC users, and OAC continuation beyond 90 days in LAAO users), and inverse probability of censoring weighting was applied to account for potential informative censoring.
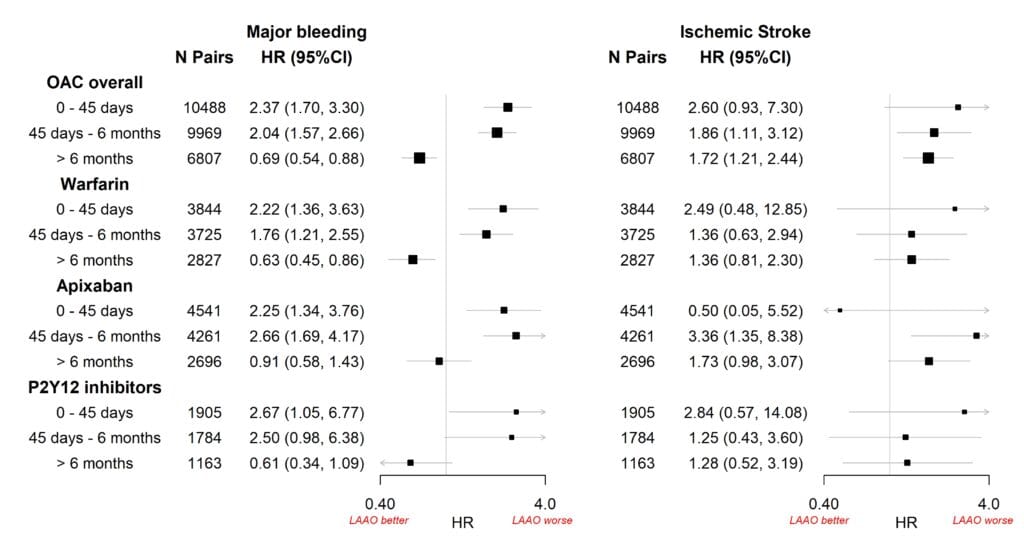
Results and Conclusions: Patients’ median age was 77; 46% were female. Compared to OAC-only users, LAAO users had a 2-fold risk of bleeding within the first 45 days (HR 2.37, 95% CI 1.70-3.30) and 45 days—6 months (HR 2.04; 1.57-2.66) post-implant, and a 31% reduced bleeding risk beyond 6 months (HR 0.69; 0.54-0.88). Additionally, LAAO users had a 70% higher risk of ischemic stroke beyond 6 months post-implant and before. This pattern was consistent across all individual OACs as well as P2Y12 inhibitors (Figure). No meaningful association between LAAO and mortality was observed over the 2-year follow-up. IPCW adjusted results remained unchanged. These findings highlight the heterogeneous effect of the LAAO device placement across outcomes and time periods following implantation, likely influenced by diverse antithrombotic regimens recommended at different stages post-LAAO.