Pharmacoepidemiology
Anticoagulant Treatment after Left Atrial Appendage Occlusion in Older Atrial Fibrillation Patients Xiaojuan Liu* Xiaojuan Liu Sebastian Schneeweiss Daniel E. Singer Jerry Avorn Edwin K. Heist Joshua K. Lin
Introduction: Left atrial appendage occlusion (LAAO) offers an alternative to oral anticoagulants (OAC) for stroke prevention in atrial fibrillation (AF) patients. In March 2015, the LAAO device received approval alongside a specific postprocedural pharmacologic regimen including OAC therapy for 45 days followed by dual antiplatelet therapy for 6 months, yet real-world data on adherence to these protocols remains limited.
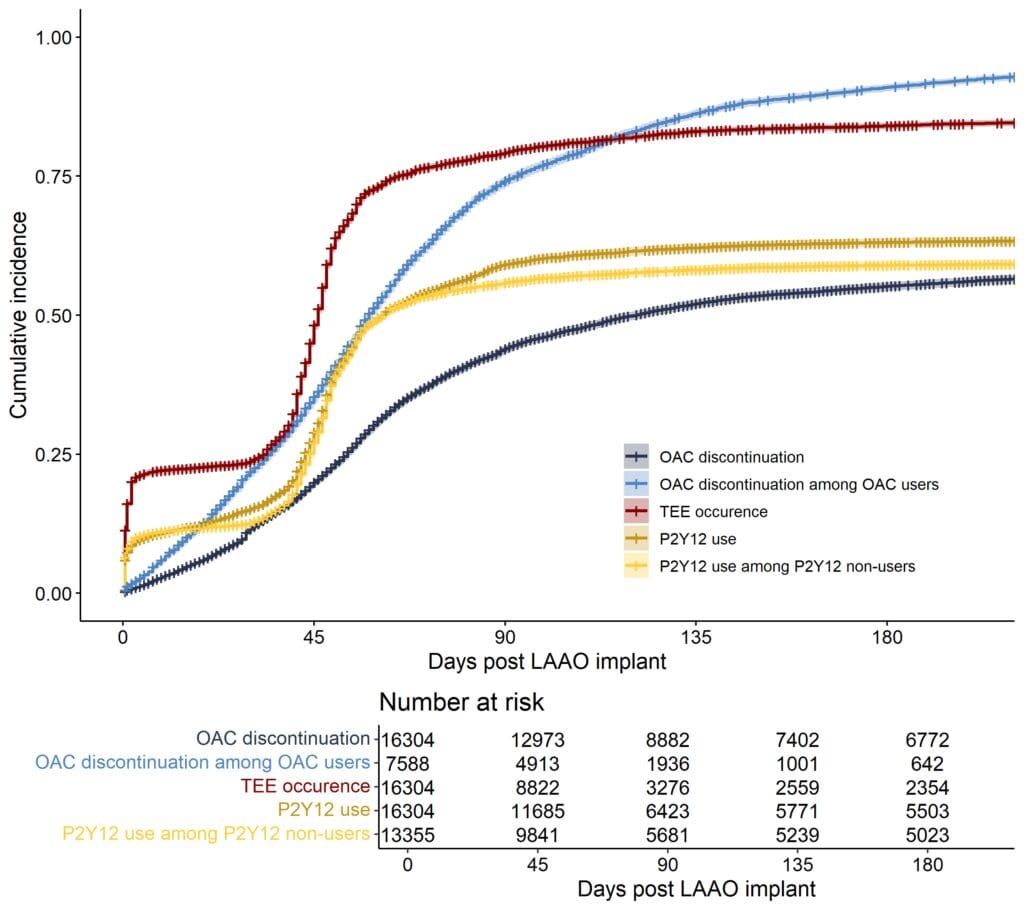
Methods: We established a cohort of 16304 AF patients who underwent first-time implantation of the LAAO device using Optum Clinformatics claims data 2015-2024. Patients aged <65 years or with a CHA2DS2-VASc score of <2 for males or <3 for females were excluded. We describe the rates of OAC discontinuation, defined as a ≥60-day gap in supply, transesophageal echocardiography (TEE) performed, and the use of P2Y12 inhibitors following implantation. Additionally, we examine the predictors of an unsuccessful occlusion and/or device-related thrombus, operationally defined as either: 1) continued OAC use following a TEE performed 30–90 days post-implant, or 2) continued OAC use beyond 90 days post-implant, regardless of whether TEE was performed.
Results and Conclusions: Among 16304 LAAO users, 3331 (20%) and 9532 (58%) discontinued OAC by 45 days and 6 months post-implant, respectively; these rates were 2675 (35%) and 6946 (92%) among 7588 patients who received OAC prior. Moreover, 10801 (66%) patients used P2Y12 inhibitors by 6 months post-implant; this rate was 8332 (62%) among 13355 prior P2Y12 non-users. TEE was performed in 7482 (46%) and 13950 (86%) patients by 45 days and 6 months post-implant, respectively (Figure). Factors associated with a higher likelihood of unsuccessful occlusion (or thrombus) included older age, Black race, and a longer duration of prior OAC use. These findings suggest moderate adherence to the LAAO postprocedural protocol. Further research is needed to assess the impact of these adherence patterns on clinical outcomes.