Methods/Statistics
Evaluating the Longitudinal Utility of the Berlin Questionnaire for Obstructive Sleep Apnea Risk: A Sequence Analysis Approach Alexandra Mueller* Alexandra Mueller David Goldfarb David Appel Rachel Zeig-Owens David Prezant
Introduction: The Berlin Questionnaire (BQ), validated cross-sectionally and widely used, identifies Obstructive Sleep Apnea (OSA) risk. Its longitudinal performance remains unexamined. We used Sequence Analysis (SA) to evaluate temporal trajectories of BQ-identified OSA risk, assess clusters with similar trajectories, and characterize cluster differences.
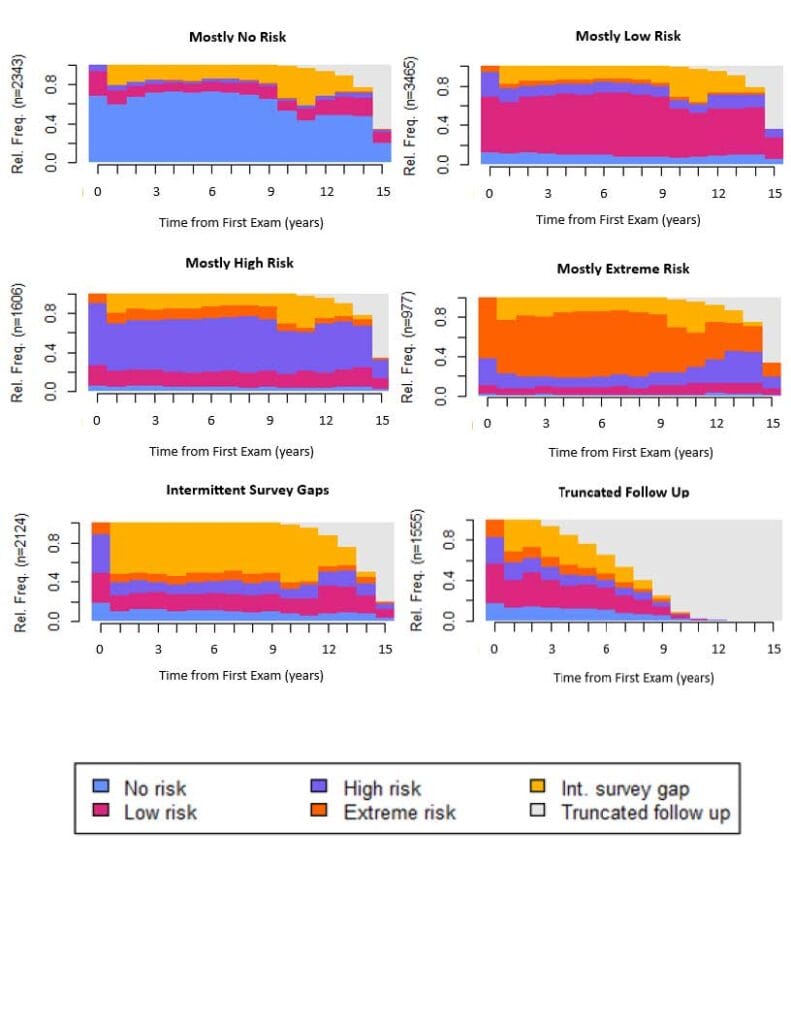
Methods: Retrospectively, we studied Fire Department of the City of New York World Trade Center Program participants who completed BQ across multiple time points from 2009-2024 starting at first survey. At each exam, participants scored into 1 of 4 categories based on the number of positive BQ domains – snoring, fatigue, blood pressure/body mass index: no-risk (NR) (0/3), low-risk (LR) (1/3), high-risk (HR) (2/3), extreme-risk (ER) (3/3). SA identified longitudinal sequences of BQ risk classifications, clustering participants with similar trajectories. We calculated risk ratios using log-binomial regression and computed p-for-trend, adjusting for age at first BQ, race, sex, and smoking status.
Results: From 12,070 participants with 3+ BQ (mean=11), we identified 6 distinct clusters: mostly NR (19%), mostly LR (29%), mostly HR (13%), mostly ER (8%), intermittent survey gaps (18%), and truncated follow up (13%). Fig. 1 shows relative frequencies of each BQ-risk category over time per cluster. Over 80% consistently scored into their cluster’s corresponding BQ-risk category >50% of surveys. Increasing risk severity cluster is associated with continuous positive airway pressure treatment authorization, notably with mostly HR and ER clusters differing significantly.
Conclusion: Most participants remained consistent in BQ-risk category over 15 years. While the BQ is only validated combining high- and extreme-risk, mostly HR and ER clusters differed, providing rationale for the use of 3 BQ risk categories in research settings. These findings suggest potential use of BQ risk as an OSA proxy in longitudinal studies.