Perinatal & Pediatric
Heat stress and placental abruption: A space–time stratified case-crossover study in Japan Shuhei Terada* Shuhei Terada Hisaaki Nishimura Naoyuki Miyasaka Takeo Fujiwara
Background: Previous studies have highlighted associations between heat stress during pregnancy and perinatal complications such as preterm birth. However, surprisingly little evidence exists regarding environmental triggers of placental abruptions, despite its significant impact on maternal and fetal mortality and morbidity.
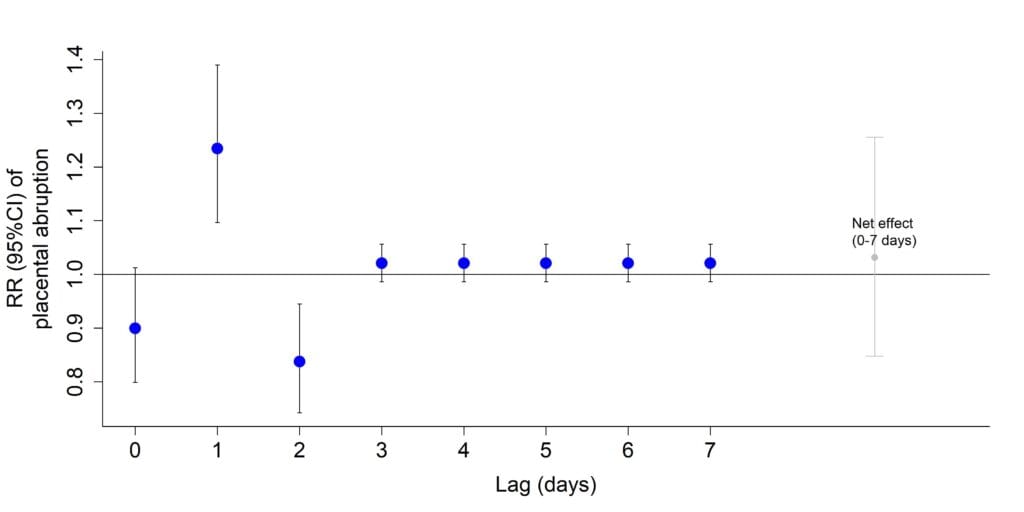
Objective: To examine whether heat stress, measured by WBGT (which incorporates temperature, humidity, wind speed, and solar radiation), is associated with an increased risk of placental abruption within the following 7 days.
Methods: We used a space–time-stratified case-crossover design with data from the Japan Perinatal Registry Network, covering daily placental abruption cases in 11 regions during the warm season (June–September) from 2011 to 2020. Heat stress was defined as daily maximum WBGT exceeding the 95th percentile of regional distributions, with data from 11 observatories across Japan. Associations were assessed using quasi-Poisson regression with distributed lag linear models over a lag period of 0–7 days. Stratified analyses were performed based on gestational week (preterm vs. term pregnancies), hypertensive disorders of pregnancy (HDP), and small for gestational age (SGA).
Results: Among 8,613 cases of placental abruption identified, heat stress was associated with an increased risk of placental abruption on lag 1 (RR: 1.23, 95% CI: 1.11, 1.39). The risk decreased on lag 2 (RR: 0.84, 95% CI: 0.74, 0.95), resulting in negligible cumulative risk over lag 0–7 due to counterbalancing effects. Similar associations were observed in preterm and term pregnancies. Higher risks on lag 1 were observed in women with HDP (RR: 1.57, 95% CI: 1.31, 1.88), and in those with SGA infants (RR: 1.47, 95% CI: 1.26, 1.73).
Conclusion: Heat stress during pregnancy was associated with an increased risk of placental abruption the day after exposure, suggesting a short-term displacement effect, particularly in women with HDP or SGA infants.