Mental Health
Suicide and Unintentional Poisoning Mortality after Involuntary Psychiatric Hospitalization: A Time-to-Event Analysis with Linked Data from Public Agencies Warren Szewczyk* Warren Szewczyk Spencer Hensley Ali Rowhani-Rahbar Alastair Matheson Isaac Rhew
Background: No studies in the United States have characterized suicide or unintentional poisoning (UP) mortality after involuntary psychiatric hospitalization (IPH). We aimed to estimate the incidences of suicide and UP death after last IPH and investigate factors associated with these outcomes.
Methods: Data for this retrospective cohort study were sourced from the New Opportunities in Health and Resilience Measures for Suicide (NO HARMS) database, which links administrative service utilization records in King County, Washington, and statewide death records. Participants included all people with ≥1 IPH order in King County from January 2016 – December 2022 (N=22,942). We used Kaplan-Meier methods to estimate incidences of suicide and UP death after last recorded IPH and Cox proportional hazards models to estimate associations of these outcomes with age, gender, race, homelessness service use, jail, a history of >1 IPHs, last IPH length of stay, and detainment order type for last IPH.
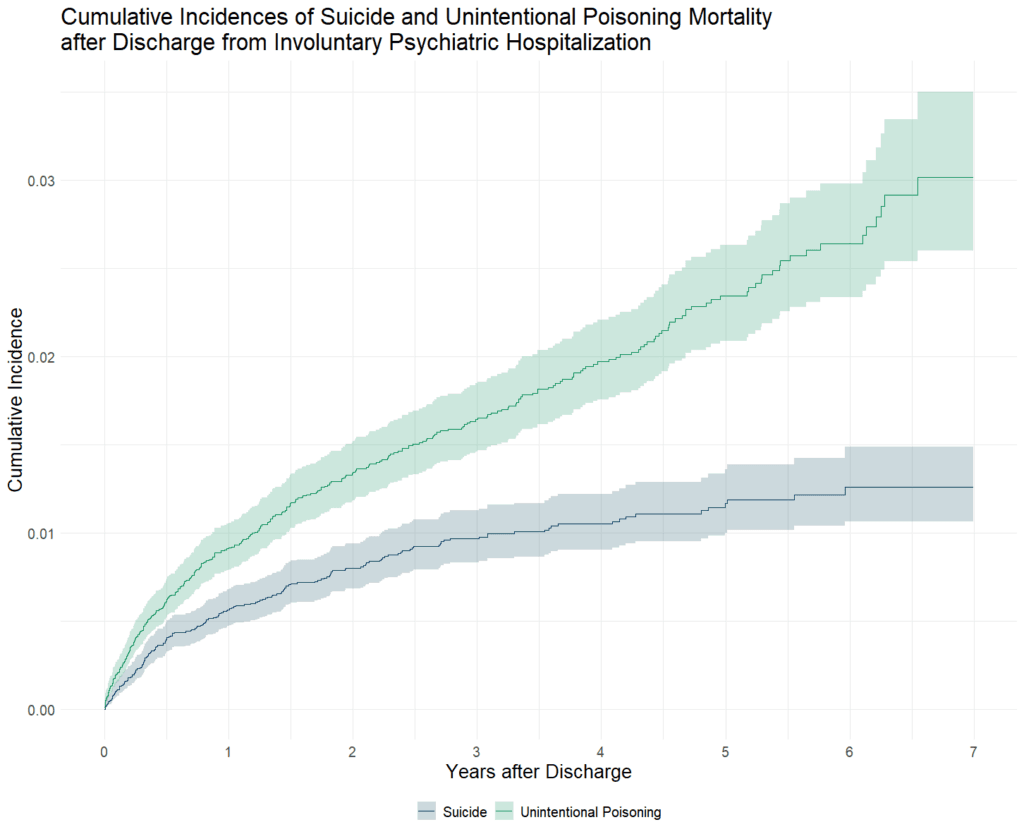
Results: The 1-year and 7-year cumulative incidences of suicide after last IPH were 0.56% (95% CI=0.47,0.68) and 1.26% (95% CI=1.06,1.48) and of UP death were 0.92% (95% CI=0.79,1.05) and 3.03% (95% CI=2.59,3.49). Asian, Black, and White racial classifications were each associated with greater risk of suicide and UP death compared to not having those classifications (all p<0.001). Male gender, homelessness service use, a jail stay before last IPH, and a history of multiple IPHs were associated with UP mortality (all p<0.05). Compared to a Danger to Others detainment order, a Danger to Self order was associated with both suicide (p<0.001) and UP death (p<0.05).
Conclusion: The cumulative incidences of suicide and UP mortality were comparable to published values for patients discharged from voluntary psychiatric hospitalization. The first year after discharge is an important period for intervention. Further research is needed to develop effective suicide and UP prevention strategies.