Neurology
Are Individuals with Diabetes Less Likely to Develop Amyotrophic Lateral Sclerosis? Mario Flores* Mario Flores Éilis O’Reilly Marianna Cortese Alpa Patel Yikyung Park Laurence Kolonel Kjetil Bjornevik Alberto Ascherio
Objective–To examine whether individuals with diabetes have a lower risk of amyotrophic lateral sclerosis (ALS) than those without diabetes.
Background–Although an inverse association between diabetes and ALS has been consistently reported in epidemiological studies, these studies have lacked information on potential confounders such as smoking and physical activity, and have not examined temporal variations in ALS risk.
Methods–We used prospectively collected data of 985,805 individuals from five US cohort studies. Individuals with diabetes at baseline were matched to those without diabetes in a 1:1 ratio according to age, sex, race, cohort, obesity, smoking status, and level of physical activity. We estimated the risk of ALS at 5, 10, and 15 years in those with and without diabetes using the Kaplan-Meier estimator. Risk ratios were obtained by dividing risk estimates. Percentile-based confidence intervals (CI) were calculated using bootstrapping.
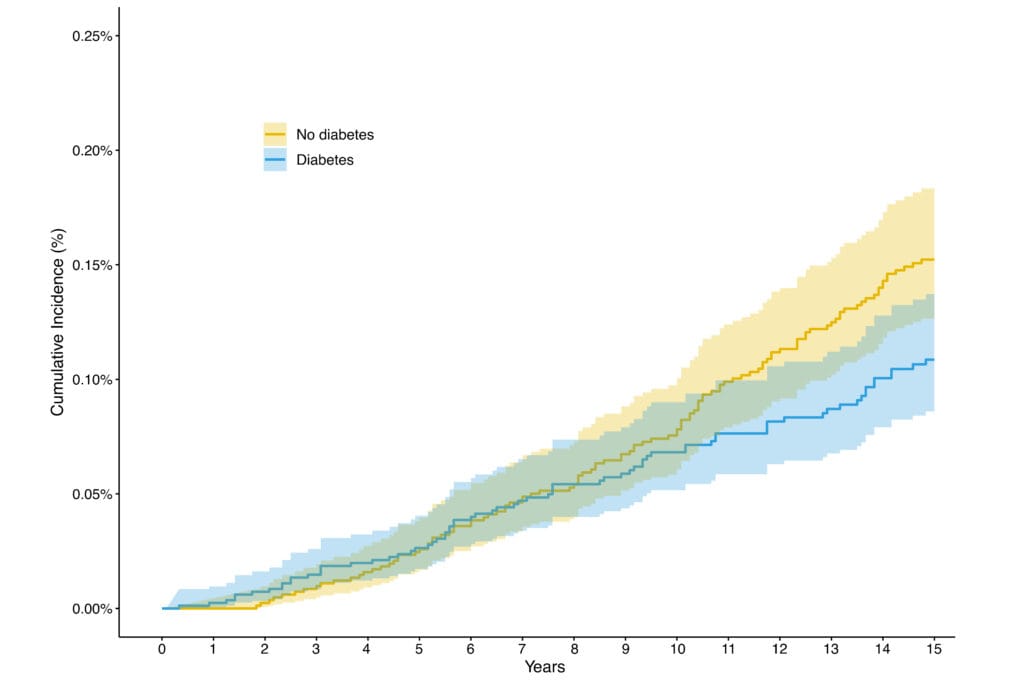
Results–This analysis included 84,066 individuals with diabetes at baseline with a mean age of 63 (SD, 6.5) years, who were matched to 84,066 individuals without diabetes; 197 individuals developed ALS during follow-up. Among those with diabetes, the estimated risk of ALS (events/10,000 persons) was 2.6 (95% CI:1.7-4.0) at 5 years, 6.8 (95% CI:5.2-9.0) at 10 years, and 10.9 (95% CI:8.6-13.7) at 15 years. The corresponding risks among those without diabetes were 2.7 (95% CI:1.7-4.1), 7.8 (95% CI:6.1-10.1), and 15.4 (95% CI:12.7-18.3). The risk ratio of ALS comparing individuals with and without diabetes was 0.98 (95% CI:0.35-1.98), 0.87 (95% CI:0.48-1.41), and 0.71 (95% CI:0.46-1.17), at 5, 10, and 15 years, respectively.
Conclusion–Individuals with diabetes appeared to have a lower ALS risk than similar individuals without diabetes; this difference increased over follow-up time but failed to reach statistical significance. The impact of prevalent user bias, competing events, and diabetes treatment will be explored in sensitivity analyses.