Aging
The Bidirectional Relationship Between Depression and Inflammation and Their Roles in Midlife Cognitive Outcomes: The CHAMACOS Maternal Cognition Study 2022-2024 Thirsten J. Stockton* Thirsten Stockton Lucia Calderon Kelsey MacCuish Katherine Kogut Kara E. Rudolph Nicholas T. Williams Norma Morga José Camacho Lizari Garcia Yesli Perez-Rocha Maria Rodriguez Monica Romero Aaron McDowell-Sánchez Marcella Warner Weihong Guo Julianna Deardorff Nina Holland Brenda Eskenazi Jaqueline M. Torres
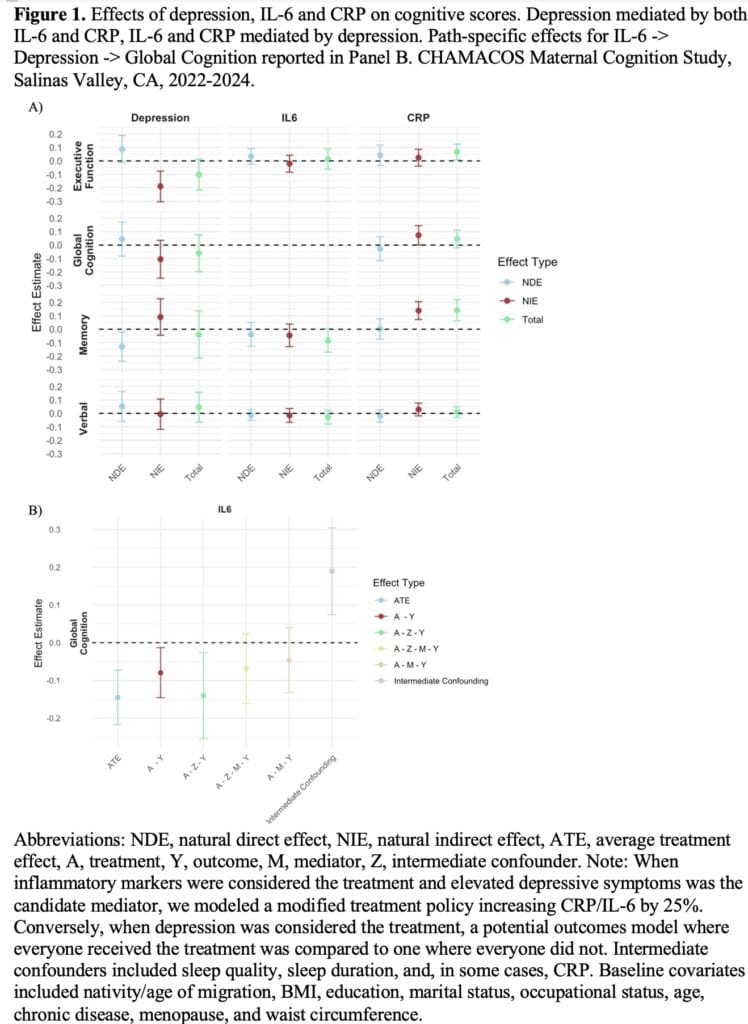
Background: Depression and inflammation share a bidirectional relationship, both being shown to influence cognition over the life course. We evaluated whether inflammation mediates the relationship between depression and cognition and, conversely, whether depression mediates the relationship between inflammatory markers and cognition in a cohort often excluded from cognitive aging research.
Methods: We used data from the CHAMACOS Maternal Cognition Study (2022-2024), which included 483 midlife Latina women from an underserved agricultural region. We measured elevated past-week depressive symptoms, log interleukin-6 (IL-6), log c-reactive protein (CRP), principal component-derived global and domain-specific cognitive scores, and socio-demographic covariates. We estimated both path-specific effects (to quantify the significance of intermediate confounding) and natural effects using a unified machine-learning approach with cross-validation. If significant intermediate confounding was observed, only path-specific effects were reported.
Results: Total and natural (in)direct effects of depressive symptoms on global cognition via inflammation were null. However, for executive function, there was a significant indirect effect via inflammation, while depression directly affected memory. (Fig 1, Panel A). Total and direct effects were null for CRP and global cognition, while indirect effects via depressive symptoms were unexpectedly protective. Significant intermediate confounding was found when estimating whether depressive symptoms mediated the relationship between IL-6 and global cognition (Fig 1, Panel B). Path-specific estimates provided limited evidence of mediation via depressive symptoms and supported a direct relationship between IL-6 and global cognition, alongside other pathways.
Conclusion: Findings highlight a complex interplay between depression, inflammation, and cognition in midlife and the need for careful evaluation of assumptions for mediation analyses.