Health Disparities
Association Between Social Risk Factors and Major Adverse Cardiovascular Events and Mortality Among Individuals with Rheumatic Conditions Leah Santacroce* Leah Santacroce Jeong Yee Jing Cui Emily Oakes Hongshu Guan Karen Costenbader Candace Feldman
Background
Individuals with rheumatic conditions are at an increased risk of experiencing cardiovascular events. Social risk factors contribute to inequities in comorbidities and adverse outcomes and may confer higher risk of Major Adverse Cardiovascular Events (MACE) in patients with rheumatic conditions.
Methods
We used data from the nationwide NIH All of Us Research Program (V7) and included adults with ≥ 2 diagnosis codes ≥30 days apart for lupus (SLE), rheumatoid arthritis (RA), and osteoarthritis (OA) 2 years pre-enrollment.
A Social Determinants of Health questionnaire was completed at enrollment. We developed social risk factor indices for economic instability and healthcare access challenges based on needs reported. Discrimination was measured with the Everyday Discrimination Scale.
The primary outcome of MACE included myocardial infarction, stroke, intervention for coronary artery disease, and all-cause mortality. Patients were followed from enrollment until their first event or end of study period.
We used multivariable Cox proportional hazard models to evaluate the associations between each social risk factor index and MACE and mortality, adjusting for age, sex, race, rheumatic disease and Deyo-Charlson Comorbidity index.
Results
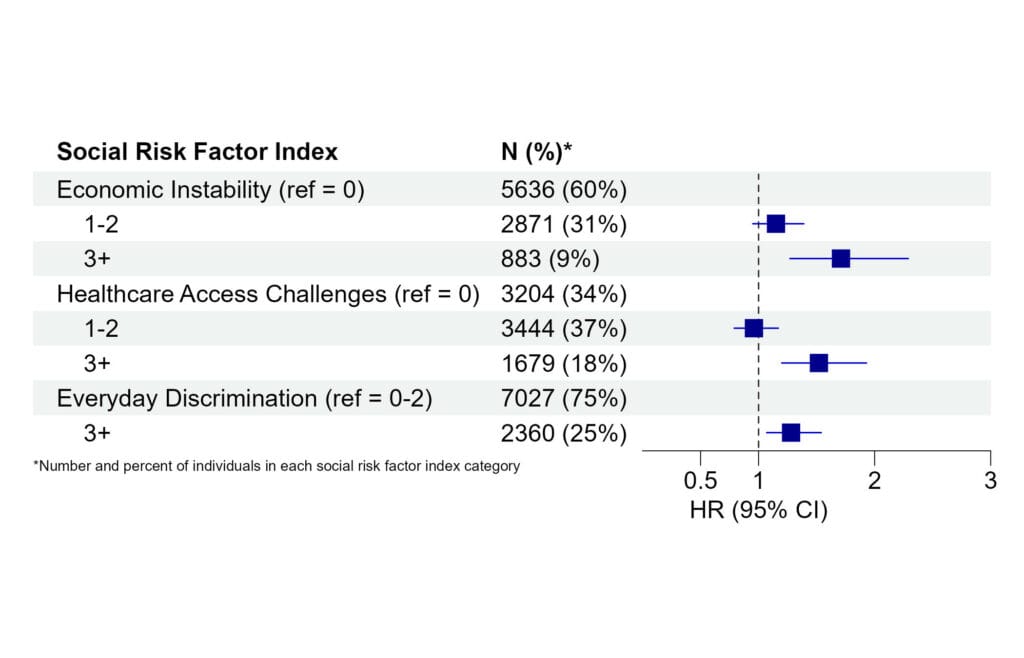
We identified 9,390 patients who met our criteria. There were 637 events, and the mean (SD) follow up time was 2.3 (1.4) years. After adjusting for covariates, individuals with 3+ economic insecurities (HR 1.86, 95% CI 1.86 – 2.43), 3+ healthcare access challenges (HR 1.52, 95% CI 1.20 – 1.93), or experienced discrimination (HR 1.28, 95% CI 1.07 – 1.54) were at higher risk of MACE compared to those without each social risk factor (Figure 1).
Discussion
In this national study, we found that higher burden of social risk factors was strongly associated with increased risk of MACE and mortality among individuals with SLE, RA, and OA. Further studies should determine whether addressing social needs reduces risk of cardiovascular events.