Global Health
Effect of an integrated newborn care kit on neonatal and maternal health outcomes: A cluster randomized controlled trial in Gilgit-Baltistan, Pakistan Daniel Farrar* Daniel Farrar Lisa G. Pell Muhammad Yasin Falak Madhani Shariq Paracha Adria Rose Diego G. Bassani Imran Ahmed Muhammad Karim Nazia Jabeen Faisal Ali Masood Ali Khan Sajid B. Soofi Monica Taljaard Rachel F. Spitzer Sifat Wali Dr. Saleemuddin Sher Hafiz Khan Zulfiqar A. Bhutta Shaun K. Morris
Introduction: Pakistan experiences very high rates of neonatal mortality (NMR). Low-cost, community-based interventions are needed to prevent newborn deaths and related morbidities. We estimated the effect of an integrated newborn care kit (iNCK) on neonatal mortality, when delivered by Lady Health Workers (LHWs) to pregnant women.
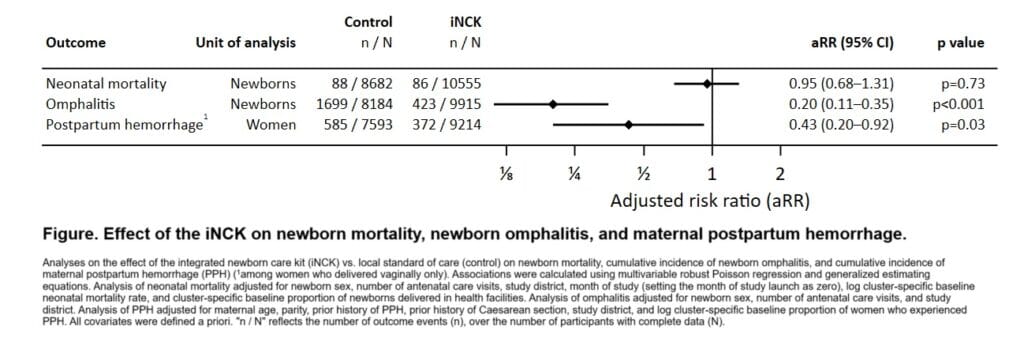
Methods: We conducted a parallel-arm, pragmatic, open-label, cluster randomized controlled trial in Gilgit-Baltistan, Pakistan from March 2022–August 2024. Clusters were randomized to the iNCK or local standard of care (control) arm. Pregnant women were delivered the iNCK and/or standard of care by LHWs during the third trimester. The iNCK included a clean birth kit, 4% chlorhexidine gel, sunflower oil emollient, ThermoSpotTM temperature indicator sticker, fleece blanket, click-to-heat warmer, three 200 µg misoprostol tablets, and pictorial guide. The primary outcome was neonatal mortality, or death within 28 days after birth. Secondary outcomes include newborn omphalitis and maternal postpartum hemorrhage. The effect of the iNCK was assessed using generalized estimating equations and multivariable robust Poisson regression.
Results: 19352 pregnant women (8723 control, 10629 iNCK) and their 19237 live-born newborns (8682 control, 10555 iNCK) were enrolled. There were 174 newborn deaths, 88 in control clusters (NMR 10.1 per 1000 live births) and 86 in iNCK clusters (NMR 8.1 per 1000 live births). Neonatal mortality was not significantly different between arms (aRR 0.95, 95% CI 0.68–1.31; p=0.73) (Figure). Cumulative incidence of omphalitis was lower among newborns in iNCK clusters (aRR 0.20 vs. control, 95% CI 0.11–0.35, p<0.001). Among women delivering vaginally, postpartum hemorrhage was less common in iNCK than control clusters (aRR 0.43, 95% CI 0.20–0.90, p=0.03).
Discussion: The iNCK reduced morbidity among newborns and women in Pakistan. We will generate policy-relevant evidence for Pakistan and other settings with high NMRs.