Big Data/Machine Learning/AI
Geospatial clustering of physician age in the US physician workforce Jag Lally* Jag Lally Ryan Crowley David M Kline Amanda Bunting
Background: We investigated geospatial clustering of physician age among physicians in 2024, focusing on how regional characteristics influence areas of high or low physician age.
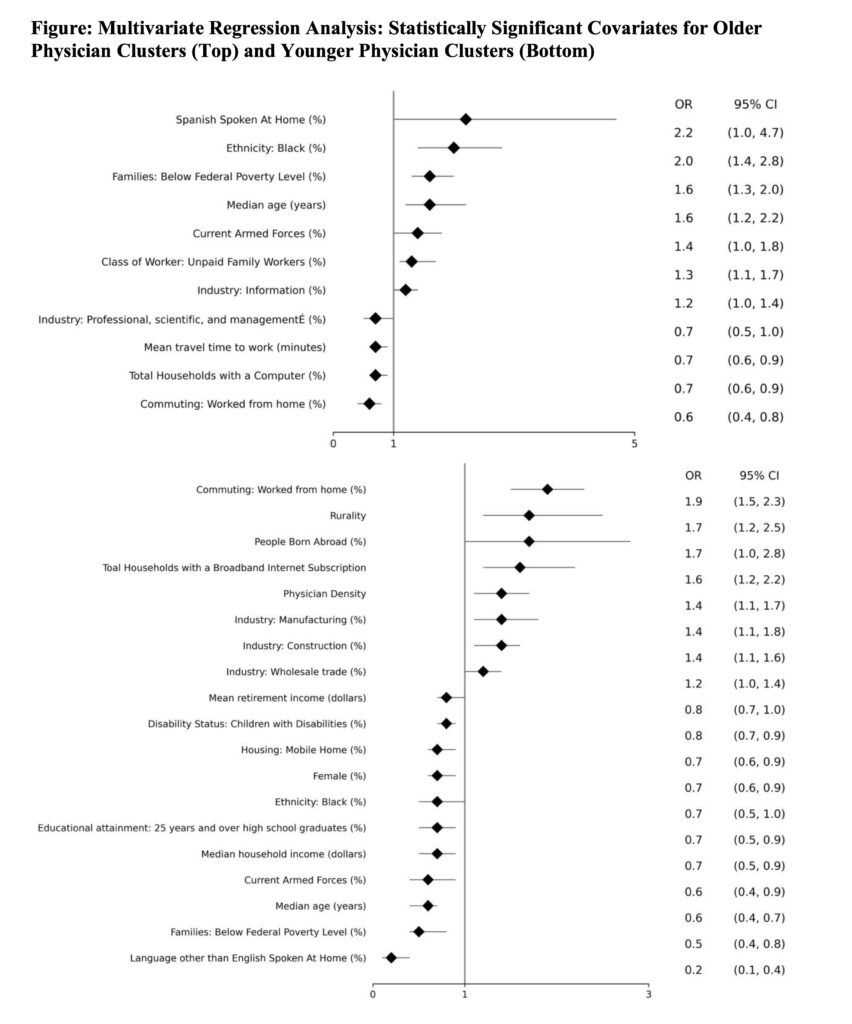
Methods: We linked the 2008-2021 Medicare Data on Provider Practice and Specialty (MD-PPAS) dataset with the 2024 Centers for Medicare and Medicaid Services (CMS) Doctors and Clinicians national downloadable file. All US physician providers with valid National Provider Identifiers (NPIs), zip code, and age data were included. We used Rural-Urban Continuum Codes (RUCCs) to measure rurality. We performed Local Indicators of Spatial Association mapping of counties which identified clusters of counties with physician ages above and below the median. Multivariate regression analyses using county-level demographic, socioeconomic, and healthcare variables from the American Community Survey (ACS) data were performed to identify factors associated with regions of older and younger physicians.
Results: The mean physician age was 52.6 years. There were clusters of high physician age in Wyoming, North Dakota, Texas, Alabama, Mississippi, and Georgia and clusters of low physician age in Washington, Utah, Colorado, Kansas, and Illinois. Most of the high age clusters were in rural counties. Counties with higher levels of Spanish spoken at home (OR: 2.2, 95% Cl: 10-4.7) and with a greater prevalence of Black residents (OR 2.0, 95% CI: 1.4-2.8) were most strongly associated with high physician ages. Counties with more individuals working from home (OR 1.9, 95% CI: 1.5–2.3) and more rural counties (OR 1.7 95% CI: 1.2–2.5) were strongly associated with low physician ages.
Conclusions: Distinct geographic clusters of older physician ages in certain counties could exacerbate healthcare access disparities as these providers age and retire. Socioeconomic and infrastructural factors may shape physician demographic patterns, and targeted interventions could aid efforts to achieve greater healthcare equity.