Health Services/Policy
Variations in Physician Age: A United States Urban–Rural Comparison Ryan Crowley* Ryan Crowley Jag Lally David M. Kline Amanda M. Bunting
Background: Individuals in rural areas often suffer from a lack of adequate health care resources. The uneven distribution of physicians between urban and rural areas could exacerbate healthcare disparities, and these disparities could be worsened as physicians age and retire. We aimed to assess whether there are regional differences in the mean age of physician providers in urban versus rural areas.
Methods: We linked the Center for Medicare and Medicaid Services’ Medicare Data on Provider Practice and Specialty (MD-PPAS) dataset with the November 2024 CMS Doctors and Clinicians national downloadable file using the National Provider Identifier (NPI). We used Rural-Urban Continuum Codes (RUCCs) as the metric of rurality with urban areas defined as RUCC codes 1-3 and rural areas defined as RUCC codes 4-9. We then identified the 20 states with the largest, statistically significant discrepancies in mean physician ages between urban and rural areas. We assessed differences in the mean age of physician providers in urban versus rural areas for states using a two-sample t-test for significance.
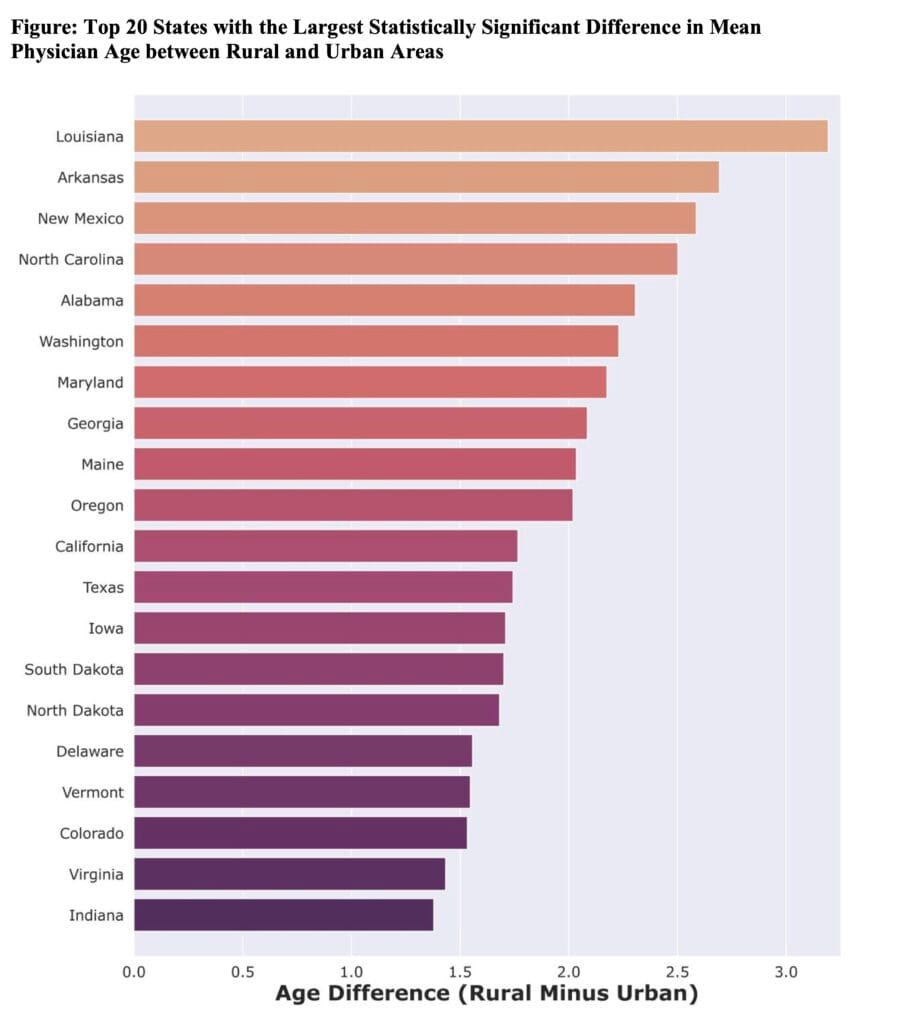
Results: Our linked cohort comprised 576,588 physicians. The average age across the US in urban areas was 52.5 years, and the average age in rural areas was 53.4 years (p-value <.00001). The states with the greatest difference in age between urban and rural areas with older providers in rural areas are Louisiana (3.2 years), Arkansas (2.7 years), and New Mexico (2.6 years). Only two states (New Jersey and New York) had statistically significant differences in age between urban and rural areas with older physicians in urban areas.
Conclusion: Physicians in rural areas are older than physicians in more urban areas, with certain states demonstrating especially large age disparities. These findings have important policy implications as aging of the rural physician workforce could exacerbate urban-rural health access disparities.