Nutrition/Obesity
Effectiveness of interventions addressing the dual burden of malnutrition in mother–child pairs Muhammad Zia ul Haq* Muhammad Zia ul Haq Javeria Mansoor Zahid Ali Memon Zohra S Lassi
The dual burden of malnutrition (DBM)—coexisting undernutrition and overweight/obesity in mother–child pairs—requires integrated “double-duty” actions. We systematically reviewed interventions targeting DBM in mother–child dyads, focusing on effectiveness, feasibility, and acceptability.
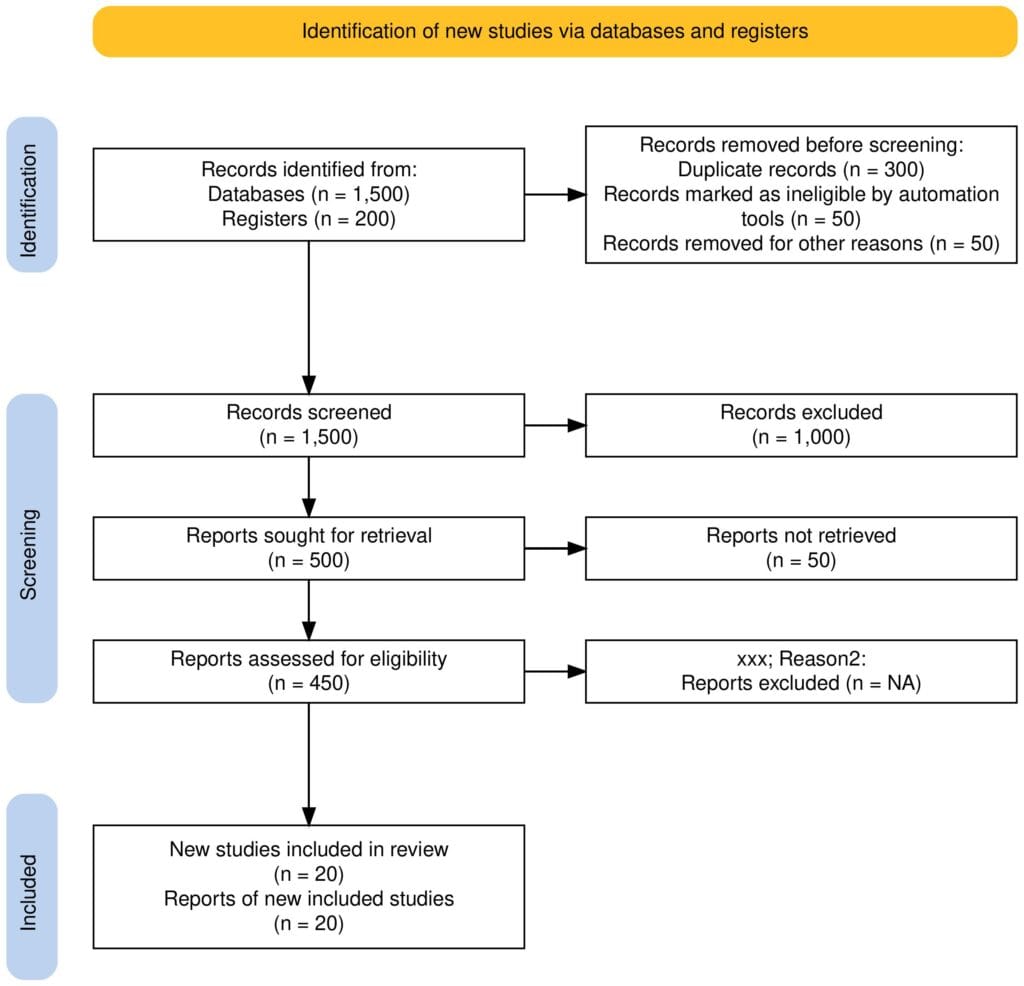
Randomized controlled trials (RCTs) were included if they enrolled mother–child pairs with discordant nutritional status (e.g., overweight mother and undernourished child). We searched major databases (PubMed, Embase, Web of Science, Scopus), screened studies independently, and assessed risk of bias using RoB 2 (RCTs) and ROBINS-I. Primary outcomes were anthropometric measures; secondary outcomes included dietary diversity, micronutrient status, and program feasibility. Data were synthesized narratively due to heterogeneity in interventions and outcome reporting.
Five key trials met inclusion criteria. Two (including the MISAME-III sub-study in Burkina Faso) evaluated micronutrient-fortified balanced energy–protein (BEP) supplements during pregnancy, reporting significant increases in maternal and newborn fat-free mass indices (Argaw et al., 2023) without raising fat mass. The Indonesian NEO-MOM trial delivered nutrition education plus motivational interviewing to overweight mothers of stunted children; mixed factorial analyses indicated improved maternal dietary behaviors and modest child height-for-age improvements. Vietnam’s PRECONCEPT trial linked higher maternal preconception BMI with improved child size at 6–7 years, underscoring the importance of maternal weight optimization. Another study from Chile (CHiMINCs) integrated nutrition counseling and breastfeeding support to control gestational weight gain and promote healthy child growth.
Double-duty interventions integrating BEP supplementation, micronutrient fortification, and behavior-change education appear feasible and beneficial for DBM in diverse settings. While improvements in anthropometry and dietary outcomes are promising, future large-scale trials should incorporate cost-effectiveness and extended follow-up to sustain progress in mother–child DBM interventions.