Reproductive
Validation of Administrative Healthcare Records for Women with Infertility Rachel Myrer* Rachel Myrer Leslie V. Farland Anna Pollack Joseph Stanford Matthew Peterson Christy Porucznik Karen Schliep
Background: Infertility affects approximately 12.1% of women and 9.4% of men in the U.S. Administrative healthcare records offer a cost-effective means to study infertility in large populations over time. However, the validity of these records to identify infertility cases remains underexplored, particularly in the U.S. where insurance coverage for fertility treatments is limited.
Objective: Validate infertility diagnoses in administrative healthcare records using self-reported time to pregnancy (TTP) as the primary reference method.
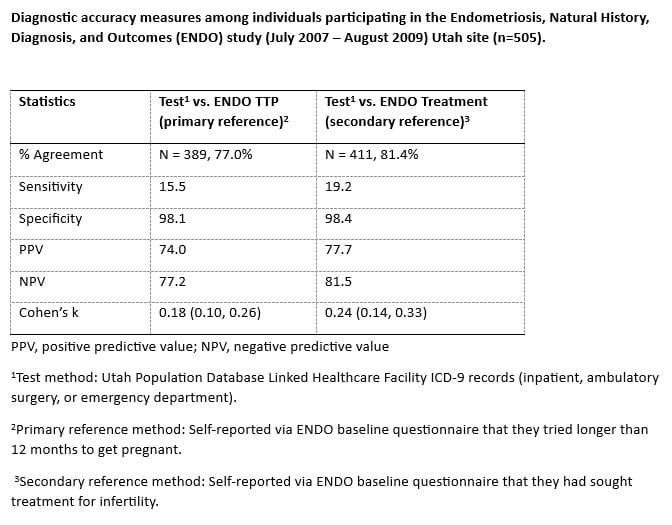
Methods: We utilized data from the Endometriosis, Natural History, Diagnosis, and Outcomes (ENDO) study (2007–2009), focusing on participants from the Utah site linked to the Utah Population Database (UPDB). The primary reference method (gold standard) for infertility was defined as having a self-reported TTP of 12 months or more. Women were infertile in the test method if they had an ICD-9 infertility diagnosis prior to or within one month of starting the ENDO study. Diagnostic accuracy was assessed using sensitivity, specificity, positive predictive value, negative predictive value, and Cohen’s kappa.
Results: The study included 505 women. The test method (UPDB) showed 77.0% agreement with the primary reference method (TTP). Sensitivity was low (15.5%), but specificity was high (98.1%). Positive predictive value was 74.0% and negative predictive value was 77.2%. Cohen’s kappa indicated slight agreement (k=0.18, CI 0.10-0.26).
Conclusions: Diagnostic codes in administrative records exhibit high specificity but low sensitivity for identifying infertility. This suggests that while these codes are reliable for confirming non-infertility, they miss many true infertility cases. Future research should address sociodemographic disparities in infertility diagnoses and incorporate additional data sources such as prescriptions, procedures, male partner records, and clinical notes to improve sensitivity and reduce false negatives.