COVID-19 Pandemic
Risk factors for progression to severe COVID: a retrospective cohort study of 994,397 persons, 2022-2024 Jorge R Ledesma* Jorge Ledesma Liyan Liu Jacek Skarbinski Joshua R Nugent
Background: Currently, providers and patients are unsure about who should receive antiviral treatment for preventing progression to severe COVID. These ambiguities arise from the following: CDC’s expansive guidelines indicate that 75% of US population is eligible for therapy, new clinical trial data showing no benefit for lower risk patients, and gaps in evidence for several risk factor-severe COVID links. A clearer understanding of who is at greatest risk for disease progression can optimize care delivery and ensure people at high risk receive treatment. We therefore aimed to describe the relationships between 30+ CDC risk factors and severe COVID.
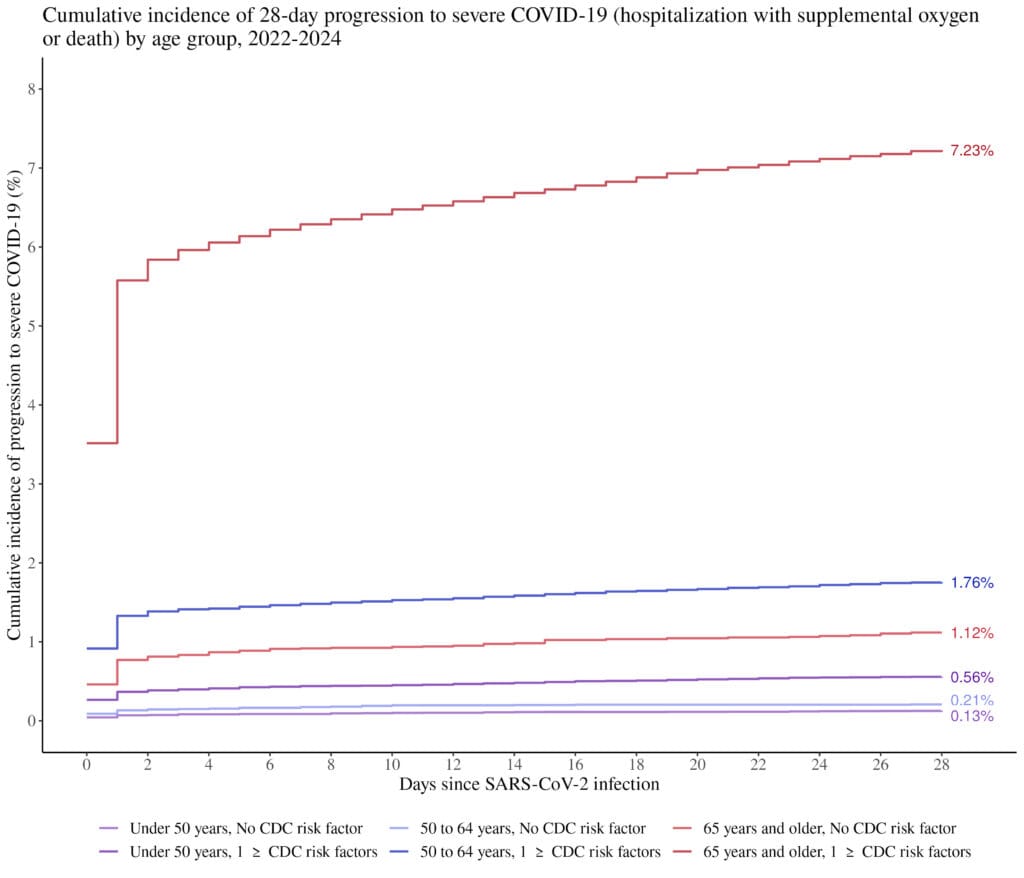
Methods: We conducted a retrospective cohort study including Kaiser Permanente Northern California (KPNC) members aged > 18 years with (1) incident SARS-CoV-2 infection and (2) > 1 year of continuous enrollment between January 2022 and December 2024. We used inverse probability weighting to create a population where treatment naïve risk (risk in the absence of future antiviral therapy) can be estimated followed by marginal standardization to derive risk differences (RD) associated with CDC risk factors and 28-day risk of severe COVID (hospitalization with supplemental oxygen or death).
Results: Among 994,397 people, 20,526 (2.06%) experienced severe COVID over 28 days: 18,991 (1.91%) were hospitalized with oxygen support and 3,542 (0.36%) died. Age was the largest risk factor (e.g., 60-69 years: RD=1.62% [95% CI 1.56-1.69]; 70-79 years: 3.12 [3.02-3.20]). Clinical risk factors with the largest excess risks were chronic lung disease (1.76% [1.63-1.91]), schizophrenia (1.71 [1.19-2.41]), and dementia (1.63% [1.50-1.76]). Risk factors with the least excess risks were mood disorders (0.56% [0.51-0.63]), asthma (0.38% [0.30-0.43]), ever smoker (0.33% [0.28-0.38]).
Conclusions: Our analysis provides new data for beginning to redefine broad treatment guidelines and optimize treatment prescribing to reduce COVID morbidity.