Big Data/Machine Learning/AI
Investigating Factors Driving Frequent Online Medical Record Access Among U.S. Adults Using Machine Learning: Analysis of the HINTS Survey Ransome Eke* Ransome Eke Joedrecka Brown Speights Shermeeka Hogans-Mathews
Introduction
The integration of online medical records (OMRs) into healthcare systems has significantly improved patient access to personal health information and communication with providers. However, disparities in the frequency of OMR use persist, driven by demographic, socioeconomic, and health-related factors. Identifying predictors of frequent OMR access is critical for addressing these inequities and improving patient engagement. This study analyzes data from the 2022 Health Information National Trends Survey (HINTS) to explore factors influencing frequent OMR access among U.S. adults.
Methodology
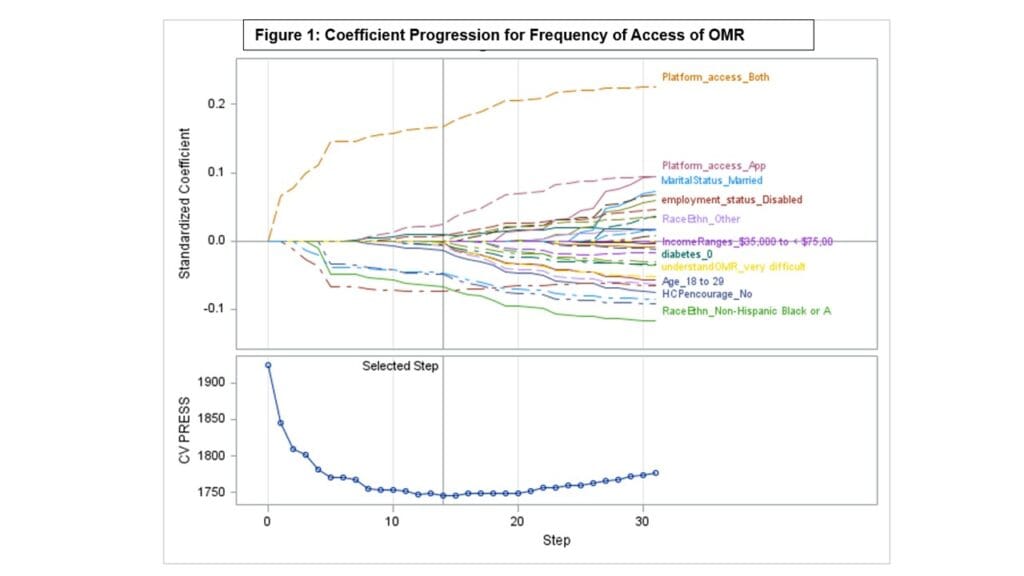
Data were derived from the 2022 HINTS survey, a nationally representative dataset examining public engagement with health information. The study included U.S. adults who reported accessing their OMRs at least once in the past 12 months. Variables such as age, gender, income, education, chronic conditions, healthcare utilization, and provider communication were assessed as potential predictors. Lasso regression was used to identify significant predictors of frequent OMR access, defined as logging in three or more times annually. Logistic regression further evaluated these predictors. Weighted analyses ensured the representativeness of the U.S. adult population.
Results
Among 2,234 respondents (weighted N = 91,439,558), 77% were frequent users of OMRs, accessing them three or more times annually. Frequent OMR use was associated with accessing records through both apps and websites (β = 0.39) or apps only (β = 0.07), as well as finding OMRs easy to understand (β = 0.23). Frequent users were more likely to be female, disabled, and Asian compared to non-Hispanic whites. Less frequent users, defined as those logging in fewer than three times annually, were more likely to include non-Hispanic Blacks (β = -0.20), those not encouraged by a healthcare provider to access OMRs (β = -0.20), individuals using only websites (β = -0.19), younger adults under 50 years, and those who found OMRs difficult to understand.
Conclusion
Ease of use, access platform preferences, provider encouragement, and demographic factors influence frequent OMR access. Targeted interventions to address barriers among underrepresented groups, such as Non-Hispanic Blacks and younger adults, are essential to ensuring equitable engagement with digital health tools.