Perinatal & Pediatric
Specific patterns of placental injury differentiate preeclampsia from other hypertensive disorders of pregnancy Marni Jacobs* Marni Jacobs Mariko Horii
Introduction: Hypertensive disorders of pregnancy (HDP) include both gestational hypertension (gHTN) and preeclampsia (PE), a severe pregnancy disorder thought to arise from abnormalities in placentation. PE may arise de novo in women normotensive prior to pregnancy, or on top of underlying pre-pregnancy chronic hypertension (superimposed PE, siPE). Although often characterized as a spectrum of disease severity, whether placental pathology differs between HDP subtypes, which may suggest differences in underlying disease etiology, is unclear. Here, we evaluate placental pathological lesions associated with HDP subtypes in a well characterized cohort.
Methods: We identified 266 chronic hypertension (cHTN), 259 gHTN, 281 siPE, and 497 primary PE cases with available placental pathology from our Obstetric Registry. Clinical diagnosis was based on current ACOG criteria, and all placentas had gross and histologic examination performed by two perinatal pathologists. Placental lesions were compared between groups using chi-square and prevalence ratios adjusted (aPR) for relevant clinical characteristics using log-binomial regression.
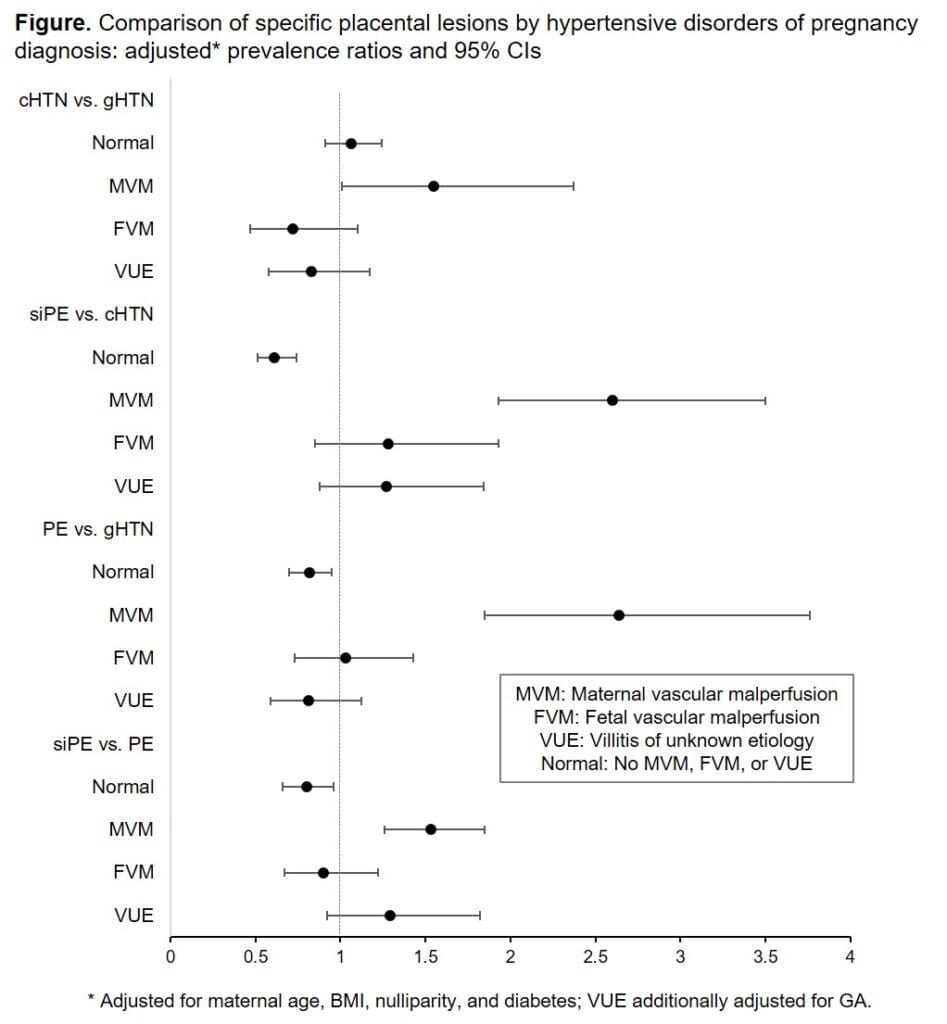
Results: Overall, few differences in placental pathology were noted between cHTN and gHTN groups, which were more likely to have normal pathology (cHTN: 58%, gHTN: 54%, PE: 36%, siPE: 44%). Maternal vascular malperfusion (MVM) was more common in both PE subtypes adjusting for maternal age, BMI, nulliparity, and diabetes (cHTN vs. gTHN: aPR 1.6, 95% CI 1.0-2.4; siPE vs. cHTN: aPR 2.6, 1.9-3.5; PE vs. gHTN: aPR 2.6, 1.9-3.8, siPE vs. PE: aPR 1.5, 1.3-1.8).
Conclusion: MVM was significantly elevated in PE compared to HTN, suggesting that MVM specifically differentiates pregnancies that progress to PE. MVM is thought to initiate in early gestation, indicating the cascade to PE is likely differentiated from HTN early in pregnancy. Future work, including molecular and cellular analysis, is needed to identify specific disease pathways.