Global Health
Changes in Maternal Mortality Ratios According to Global Health System Levels Chaoyang Li* Chaoyang Li Endang Handzel Patricia Richter
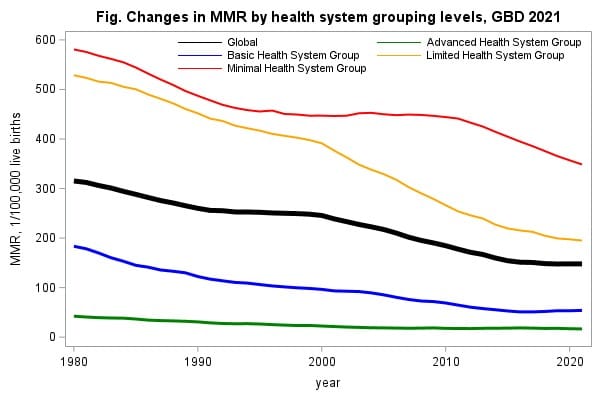
Maternal mortality is the primary reason for death among women of reproductive age worldwide. Sustainable Development Goal 3 sets a 2030 deadline to reduce the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births. This study aims to assess changes in MMRs using data from the 2021 Global Burden of Diseases Study. We included direct and indirect deaths during pregnancy, within 6 weeks of delivery, late maternal deaths up to 1 year after delivery, and HIV-related deaths aggravated by pregnancy in women of reproductive age (15-49 years). We first compared annual changes in overall and cause-specific MMRs between 1980-2000 (Period I) and 2001-2021 (Period II) and then compared the differences in two periods across four health system grouping levels (advanced, basic, limited, and minimal). We used a Generalized Estimating Equations model to account for the autocorrelation of the response variable and to test the differences in annual MMR changes between two periods across health system levels. Overall, MMR decreased by 22.1% in Period I and by 39.8% in Period II. The largest decreases were observed for maternal abortion and miscarriage (-35.2% in Period I, -56.5% in Period II) and maternal hemorrhage (-25.1% in Period I, -54.7% in Period II). Countries with advanced, basic, and minimal health systems experienced greater decreases in annual MMRs in Period I than Period II (all P<0.001). In contrast, countries with limited health systems exhibited greater progress during period II. Although other direct maternal disorders and indirect maternal deaths had increased across all health systems levels from 2000-2021, maternal hemorrhage remained the leading cause of maternal mortality globally. Despite significant improvement in MMRs, disparities persist with limited and minimal health systems exhibiting disproportionately high MMRs as of 2021. Health systems strengthening needs to be prioritized to combat maternal hemorrhage in resource-poor settings.