Perinatal & Pediatric
Placental angiogenic biomarkers in relation to prenatal bisphenol and phthalate exposure Eleanor Medley* Eleanor Medley Emma Spring Mia Charifson Sarah Adelman Yelena Afanasyeva Eunsil Seok Kurunthachalam Kannan Shilpi Mehta-Lee Whitney Cowell Linda Kahn
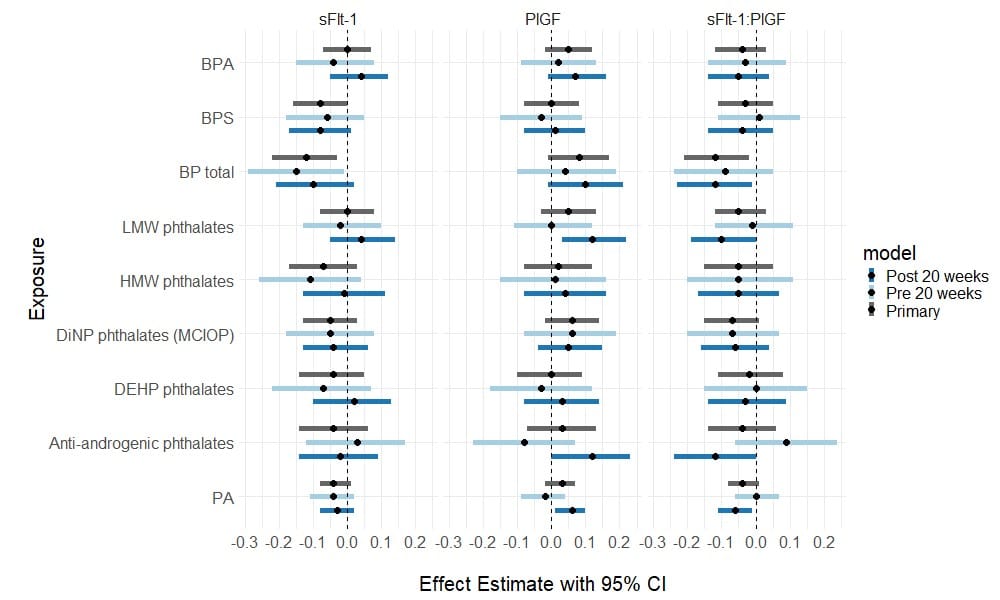
Placental growth, including the creation and expansion of blood vessels, is regulated by the concentration gradients of numerous growth factors and hormones. The development of placental vasculature has implications for both fetal and maternal health, as the vessels deliver nutrition to the fetus and regulate maternal blood pressure. Placental growth factor (PlGF) is a vascular endothelial growth factor (VEGF) hormone that promotes vasculogenesis and angiogenesis in the placenta. Soluble fms-like tyrosine kinase-1 (sFlt-1) binds to and inhibits VEGFs, preventing angiogenesis. An elevated ratio of sFlt-1:PlGF in maternal serum is predictive of preeclampsia. Exposure to two classes of ubiquitous endocrine-disrupting chemicals, bisphenols and phthalates, has also been previously linked to preeclampsia development. We investigated the relation of urinary concentrations of bisphenols and phthalate metabolites, measured up to three times during pregnancy, with serum concentrations of sFlt-1, PlGF, and their ratio in the New York University Children’s Health and the Environment Study. Linear mixed models with random intercepts were utilized to analyze up to three measurements of PlGF and sFlt-1, adjusted for gestational age at the time of serum collection. We found that the molar sum of bisphenols BPA and BPS was associated with lower sFlt-1 (-0.12, 95% CI: -0.22, -0.03), higher PlGF (0.08, 95% CI: -0.01, 0.17), and a lower sFlt-1:PlGF ratio (-0.12, 95% CI: -0.21, -0.02). No statistically significant associations were observed with six phthalate metabolite groups. The unexpected relationship between prenatal bisphenol exposure and lower sFlt-1:PlGF, possibly due to the estrogenicity of bisphenols, warrants further investigation. These results suggest that the effect of these endocrine-disrupting chemicals on placental health may be more complicated than what is currently understood through these biomarkers.