Cardiovascular
Impact of Blood Flow Patterns on Cardiac Surgery Outcomes: Pulsatile vs Non-Pulsatile Flow Ayse Ulgen* Ayse Ulgen Ercan Kahraman Sirin Cetin
Non-physiological blood flow during cardiopulmonary bypass (CPB) may contribute to postoperative complications. This study evaluates pulsatile vs non-pulsatile flow impacts on cardiac surgery outcomes.
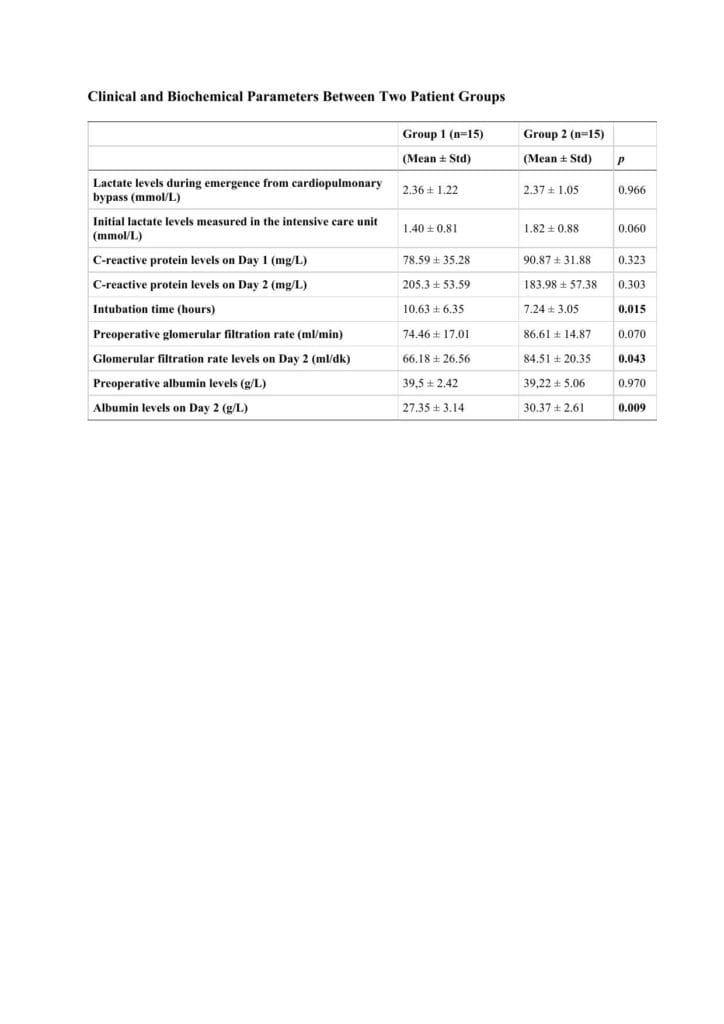
30 coronary artery bypass patients at Amasya University, Turkey, were retrospectively assigned to non-pulsatile or pulsatile CPB flow. Mean age: 61±11 years, 62% male. The following were compared: (1) Lactate levels at CPB onset and in intensive care unit (ICU) (2) Intubation duration, CRP levels (postop days 1-2); (3) pre/postop albumin and GFR level using 2-tailed t-test or Wilcoxon Rank Sum Tests.
No significant preop GFR/albumin differences (p>0.005) (Cl: 0.19-1.36 and -32.11;-9.62) was observed. Postop day 2: pulsatile group had higher GFR/albumin (p<0.005) ( Cl -2,07-;-3.04) levels. Pulsatile group had shorter intubation times (p<0.005) (Cl 0.65-.5.89). No significant differences in lactate levels during CPB/ICU or postop CRP (p>0.005) (Cl -33.51;-1.48) was observed.
Pulsatile flow positively influenced recovery post-coronary bypass. Debate continues on pulsatile vs non-pulsatile flow effects on ICU stay, morbidity, mortality. Pulsatile flow may optimize organ perfusion, enhancing hemodynamic stability. A Turkish study found preop low albumin increased post-cardiac surgery renal replacement need. Further research on pulsatile flow’s physiological benefits could inform strategies to prevent organ failure in critical patients. This study aligns with previous research showing pulsatile perfusion’s benefits. Pulsatile flow preserves microcirculation better than non-pulsatile, potentially reducing systemic inflammation during CPB. High lactate (≥4 mmol/L) during CPB correlates with increased postop morbidity/mortality. While this study found no significant lactate differences, monitoring remains crucial. Pulsatile flow’s higher circuit pressures may increase hemolysis risk, requiring careful management. Future research should standardize pulsatile flow definitions and explore its impact on specific patient subgroups.