Reproductive
Associations Between Maternal Injury and Adverse Maternal Outcomes Allison Musty* Allison Musty Elizabeth T. Jensen David Stamilio Asma M. Ahmed
Background
Maternal injury affects 6-8% of pregnancies and is associated with perinatal complications. Variation of associations by injury characteristic is underexplored. We estimated associations between maternal injury and adverse maternal outcomes.
Methods
In a retrospective cohort study using electronic health record data at Atrium Health Wake Forest Baptist (2018-2024 births), we identified maternal injury using ICD-10-CM diagnosis codes. Injury was stratified by mechanism (transport accident, fall, other unintentional, intentional), trimester, location (abdominal, non-abdominal), and severity (severe: Abbreviated Injury Scale≥2). Time-varying Cox proportional hazards models estimated associations between injury and severe maternal morbidity (SMM), stillbirth, cesarean delivery, and placental abruption, identified using ICD-10-CM diagnosis and procedure codes. Follow up spanned 20 weeks gestation to outcome occurrence, delivery, or 43 days postpartum for SMM.
Results
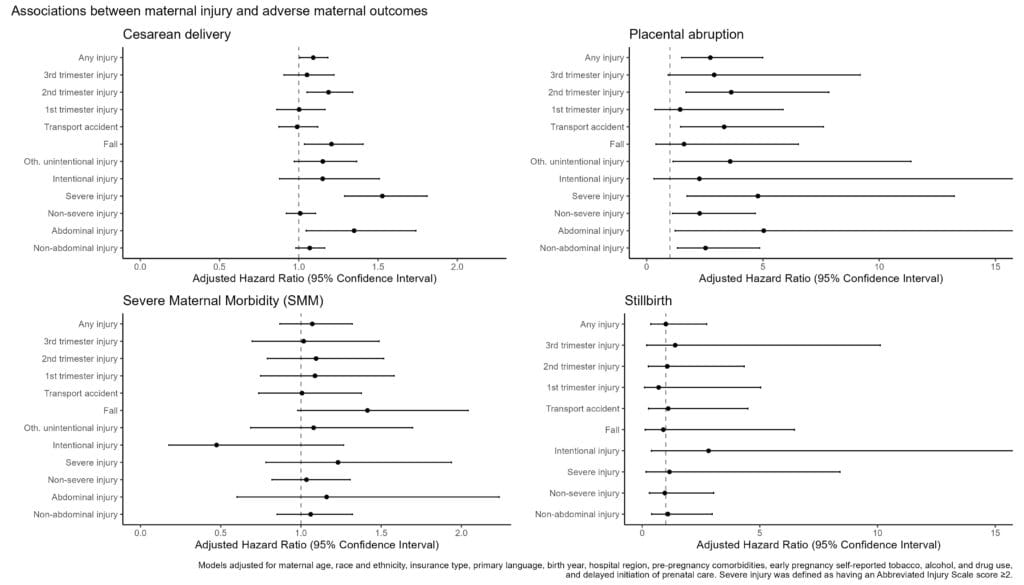
Among 58897 deliveries, 3.1% had maternal injury. SMM, stillbirth, cesarean delivery, and placental abruption affected 4.6%, 0.2%, 35%, and 0.3%, respectively. The Figure shows associations between outcomes and maternal injury. Injury was associated with increased risk of cesarean delivery (hazard ratio [HR] 1.09, 95% CI 1.01-1.18), especially from falls (HR 1.21, CI 1.04-1.41), and placental abruption (HR 2.74, CI 1.50-4.99), especially from transport accidents (HR 3.33, CI 1.46-7.61). Second trimester, severe, and abdominal injury increased risk of these two outcomes (e.g., severe injury cesarean delivery risk: HR 1.53, CI 1.29-1.81 v. non-severe: HR 1.01, CI 0.92-1.11). Injury was not associated with SMM or stillbirth.
Conclusions
Maternal injury was associated with increased risk of cesarean delivery and placental abruption, particularly for second trimester, severe, and abdominal injury. These findings may inform post-injury clinical care, focusing on pregnancies most at risk for these outcomes.