Reproductive
Pregnancy Testing Behavior in a Prospective Cohort of North American Pregnancy Planners Alexandra Sundermann* Alexandra Sundermann Anne Marie Jukic Kenneth Rothman Lauren Wise
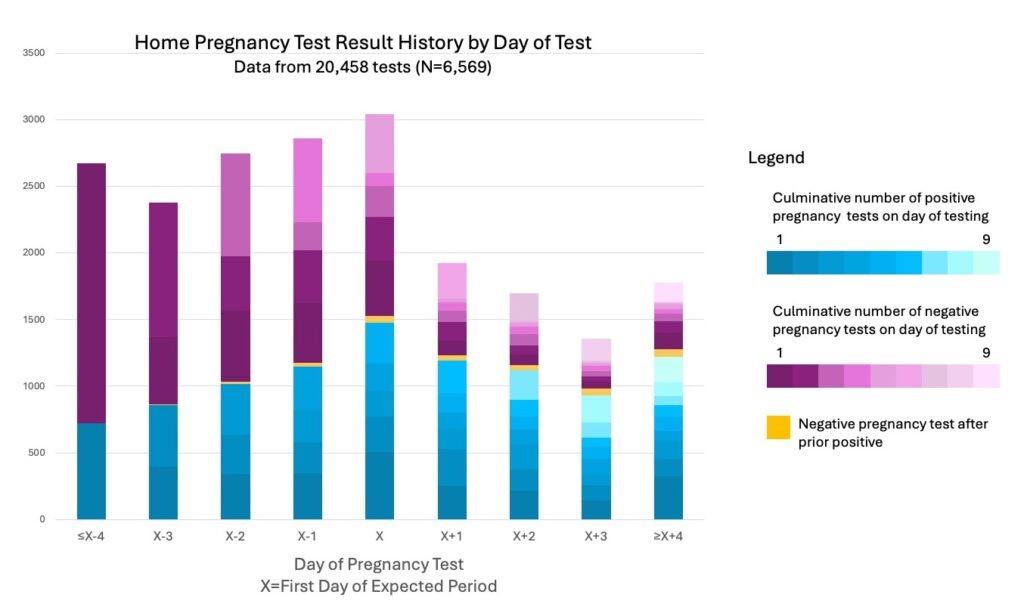
Home pregnancy testing is linked to timing of pregnancy detection and, subsequently, lifestyle modifications and eligibility for study entry in cohorts of pregnancy health. Yet, little is known about the timing and frequency of home pregnancy testing among individuals who are trying to conceive. In PRESTO (Pregnancy Study Online), a prospective cohort study of North American preconception pregnancy planners (2018-2024), participants reported day-specific information about whether they tested for pregnancy and the result of each test from four days before the day of expected menstruation through four days after. We analyzed data from the first cycle after enrollment, which included 20,458 individual tests across 6,569 unique participants. The median number of home pregnancy tests used was two (inter-quartile range [IQR]: 1, 4); 9% of participants reported testing every day within the queried range. Forty percent of participants reported testing more than four days before their expected period, whereas 26% waited to test until the day of their expected period or later. Almost half of participants had at least one positive pregnancy test (49%, n=3,241) and 60% of participants with a positive result repeated testing at least once (median number of positive tests: 2; IQR: 1, 4). We observed a range of pregnancy testing intensity, with some participants testing only once and others testing every day, even after a positive test (Figure). Participants with a history of miscarriage were more likely to be early, frequent testers compared with their counterparts (risk ratio adjusted for maternal age and parity 1.26, 95% confidence interval 1.14, 1.39). Young maternal age and increasing parity were also associated with earlier initiation of testing and more frequent testing. A deeper understanding of real-world home pregnancy test behaviors will inform quantitative assessment of biases related to timing of study entry in early pregnancy cohorts.