Mental Health
The Effects of Daylight Saving Time Clock Changes on Mental and Physical Health Outcomes in Primary and Secondary Care in England Melanie A. de Lange* Melanie A. de Lange Kate Birnie Rebecca C. Richmond Chin Yang Shapland Sophie V. Eastwood Kate Tilling Neil M. Davies
Introduction: The effects of daylight saving time (DST) transitions on health are the subject of intense debate, with the current literature fairly mixed. Few studies have looked at the effect on the health system as a whole and evidence from England is scarce. We aimed to explore the effects of the DST transitions on a range of health outcomes in a large dataset of linked English primary and secondary care records.
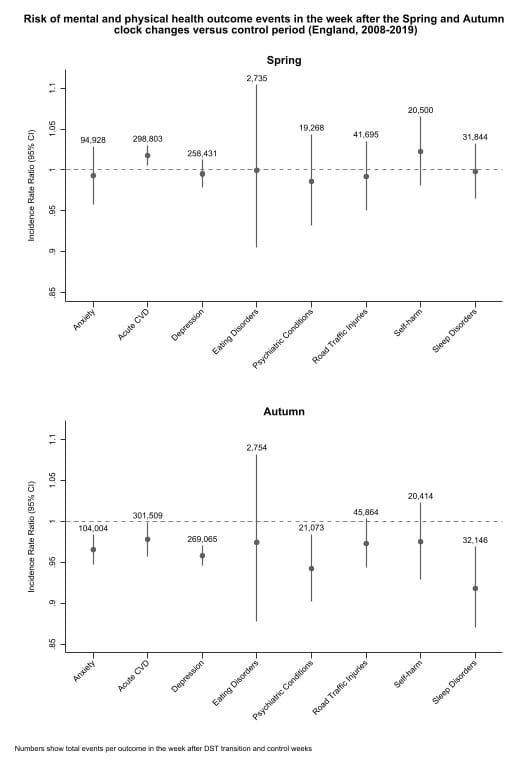
Methods: We used primary care records from the Clinical Practice Research Datalink (CPRD) Gold database linked to hospital admissions and emergency care visits. Patients were included if they had a code for acute cardiovascular disease (CVD), depression, road traffic injury, anxiety, self-harm, eating disorder or sleep disorder in their primary or secondary care record, or a code for a psychiatric condition in emergency care, in the 8-week period surrounding the Spring or Autumn clock changes between 2008 and 2019. Negative binomial regression models, adjusted for day of the week and region (and Easter weekend in Spring), compared event rates in the week after the clock changes to the control period (4 weeks before the transitions and weeks 2-4 after).
Results: In total 683,809 patients and 1,564,532 events were included in the study. In Spring we found an increase in acute CVD events in the week after the clock change (Incidence Rate Ratio: 1.02, 95%CI 1.01-1.03). In the week after the Autumn transition we found a decrease in acute CVD (IRR 0.98, 95%CI 0.96-0.999), depression (IRR 0.96, 95%CI 0.95-0.97), anxiety (IRR 0.97, 95%CI 0.95-0.98), psychiatric conditions (IRR: 0.94, 95%CI 0.90-0.98) and sleep disorders (IRR 0.92, 95%CI 0.87-0.97).
Conclusions: The Spring DST transition (when the clocks move forward an hour) was associated with an increase in acute CVD events. Meanwhile, the Autumn transition (when the clocks go back an hour) was associated with a reduction in acute CVD, sleep disorders and some mental health conditions.