Health Disparities
Socioeconomic Disparities in Temperature-related Illness Incidence: Evidence from Korea, 2014–2023 Soomin Kim* Jin Yong Lee Soomin Kim Bomi Lee Hyemin Jung
Introduction Climate change significantly impacts public health, with its effects being particularly pronounced among socioeconomically vulnerable populations. Korea’s healthcare system offers a unique model for evaluating Socioeconomic health disparities, with National Health Insurance (NHI) covering high- and middle-income groups and Medical Aid (MA) targeting low-income populations. This study analyzed the incidence rates of heat- and cold-related illnesses in Korea from 2014 to 2023 to evaluate between NHI and MA.
Methods From 2014 to 2023, the National Health Insurance claims data were used to identify patients treated for heat-related illnesses (ICD-10: T67, T69.7) and cold-related illnesses (ICD-10: T33-T35, T68, T69.0-T69.1, T69.8-T69.9) under NHI and MA. Population data for NHI and MA were obtained from Statistics Korea to serve as denominators for calculating incidence rates. Differences in incidence rates between the two groups were analyzed using ANOVA, and trend in absolute disparities over time were assessed using simple linear regression.
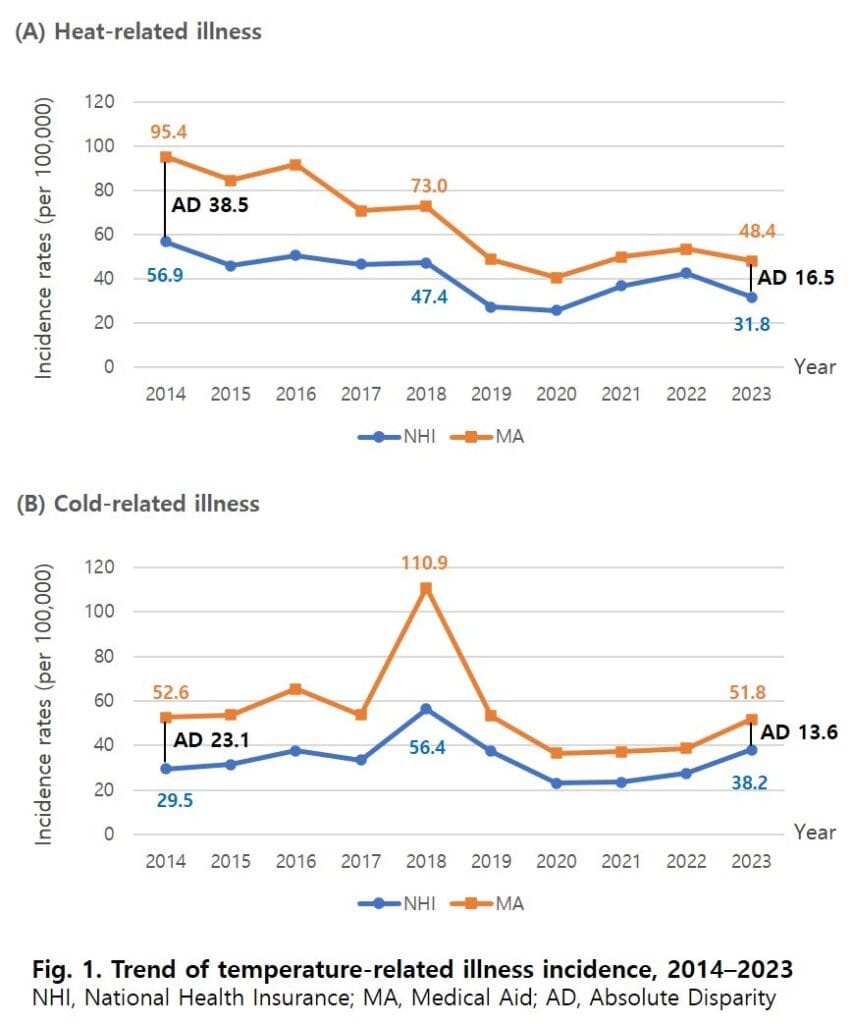
Results There were 220,339 patients with heat-related illnesses from 2014 to 2023. The average incidence rate of heat-related illnesses was 27.9 per 100,000 population for NHI and 52.4 for MA, with a difference of 24.5 (p<0.0001). The absolute disparity in heat-related illness incidence rates decreased by an average of 3.4 per 100,000 annually (p=0.0002, adjusted R-square=0.8). There were 180,971 patients with cold-related illnesses over the past decade. The average incidence rate of cold-related illnesses was 34.2 per 100,000 population for NHI and 55.8 per 100,000 for MA, with a difference of 21.6 (p=0.0005). Although the absolute disparity in cold-related illness incidence rates showed a decreasing trend of 1.8 per 100,000 annually, it was not statistically significant (p=0.2, adjusted R-square=0.07). Throughout the study period, MA consistently higher incidence rates for both illnesses compared to NHI.
Conclusions Socioeconomic disparities in heat-related illnesses have significantly improved over time; however, the improvements in cold-related illnesses have been minimal and statistically insignificant. Moreover, MA remain at a higher risk of temperature-related illnesses, likely due to environmental vulnerabilities such as inadequate access to heating and cooling resources. This study highlights the need for tailored policies that integrate welfare and healthcare services, such as expanded support for heating and cooling resources for low-income populations and the establishment of community-based emergency response systems to address extreme weather events like heatwaves and cold waves, to mitigate health disparities caused by climate change.
Disclosure of Interest: None Declared
Keywords: Heat stress disorders, cold injury, climate change, health inequalities