Cancer
Temporal patterns of uterine and ovarian cancer incidence rates in Utah after correcting for gynecologic surgeries Britton Trabert* Britton Trabert Claire E. Dunlap Jennifer A. Doherty Jessica N. Sanders Lori M. Gawron Robert L. Dood Britton Trabert
Background: Registry-based gynecologic cancer incidence rates may underestimate disease burden since the denominator includes individuals who have undergone hysterectomy or bilateral salpingo-oophorectomy (BSO), which dramatically reduce susceptibility to uterine or ovarian cancer, respectively.
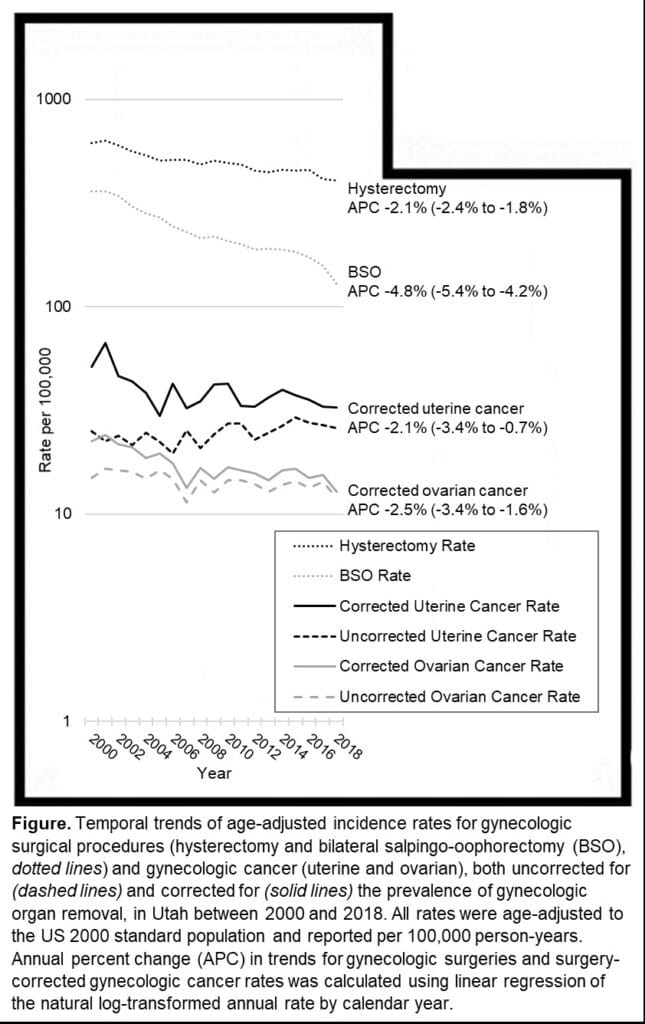
Methods: Gynecologic surgical procedures (2000-2018) were identified in the Utah Population Database (UPDB) using ICD-9/-10 and CPT codes. Procedures were categorized as any hysterectomy (with/without BSO) or any BSO. Prevalence estimates were derived using standard formula, where duration was defined as the median age at the procedure for each 5-year category subtracted from Utah’s female life expectancy (82.1 years). Uncorrected uterine and ovarian (including fallopian tube and primary peritoneal) cancer rates for Utah were obtained from SEER for the same period. To estimate corrected annual cancer rates, we subtracted prevalent surgical procedures from the age-specific denominators for Utah and recalculated rates. All rates were age-adjusted using the US 2000 standard population. Annual percent change (APC) was calculated using linear regression.
Results: Hysterectomy and BSO incidence rates decreased over time (Figure). Uncorrected uterine cancer incidence rates fluctuated between 22.4 and 26.4 cases per 100,000 from 2000-2018. After adjustment of the denominator to account for individuals no longer at risk due to hysterectomy, corrected rates showed a declining trend from 51.4 in 2000 to 32.6 in 2018 (APC -2.1%, 95%CI 3.4 to -0.7%). Uncorrected ovarian cancer rates were 14.9 per 100,000 in 2000 and 11.9 in 2018. Corrected ovarian cancer incidence rates decreased over time from 22.5 in 2000 to 12.9 in 2018 (-2.5%, -3.4 to -1.6%).
Conclusion: The differences in magnitude between the uncorrected and corrected incidence rates for ovarian and uterine cancer in Utah highlight the importance of refining population denominators to exclude individuals no longer at risk.