Health Disparities
Structural Determinants of Medical Mistrust Among Transgender Women of Color: A Mixed Methods Analysis of the TURNNT Cohort Alexander Furuya* Alexander Furuya Jenesis Merriman Adam Whalen Asa Radix Su Hyun Park Jessica Contreras Roberta Scheinmann Denton Callendar John A. Schneider Krish J. Bhatt Dustin Duncan
Background: Medical mistrust is associated with lower healthcare utilization among marginalized populations, including transgender women of color. However, medical mistrust as a construct has often placed the onus of blame on the individual or the community, rather than on systems and structures. We investigated whether structural factors, such as medical mistreatment and lack of access to transgender care, were causes of medical mistrust.
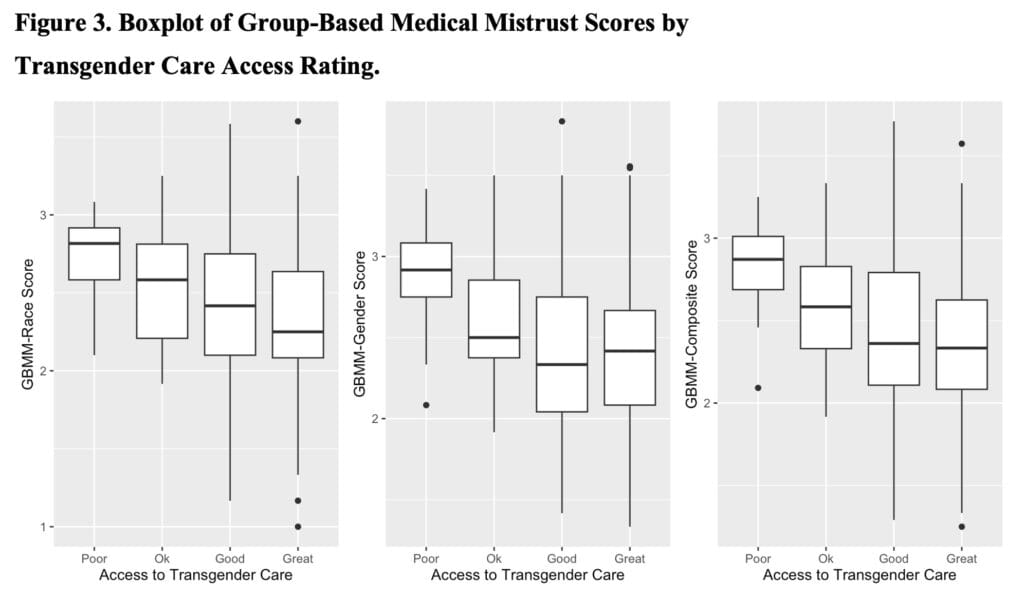
Methods: We used mixed methods to triangulate the structural determinants of medical mistrust using survey data from 193 transgender women of color living in New York City. For the quantitative analysis, we conducted t-tests and ANOVA to assess the association between our exposures (medical mistreatment and access to transgender care) and outcome (medical mistrust). We measured medical mistrust using two Group-Based Medical Mistrust (GBMM) scales, one regarding perception of medical mistrust among people of color and one regarding perception of medical mistrust among transgender women. For the qualitative analysis, we coded open-ended survey data from the participants regarding their trust towards medical institutions.
Results: We found those who had experienced discrimination in healthcare had higher levels of medical mistrust measured using both GBMM scores. Additionally, those who rated poorer access to transgender care had higher levels of medical mistrust. The open-ended survey questions corroborated these results, with many participants stating that their negative experiences with the healthcare system caused them to have distrust in medical institutions.
Conclusion: Among transgender women of color, intersecting systems of power within the healthcare setting caused these individuals to have medical mistrust. Addressing medical mistrust should not be targeted at the individual level, but rather at the structural level.