COVID-19 Pandemic
Outcomes and multimorbidity among children with neurologic and neurodevelopmental disorders hospitalized for COVID-19: The Canadian Immunization Monitoring Program Active (IMPACT) Daniel Farrar* Daniel Farrar Ryan Huang Elizabeth Donner Julie Bettinger Aaron Campigotto Costanza di Chiara Olivier Drouin Joanne Embree Scott Halperin Tajdin Jadavji Kescha Kazmi Charlotte Moore Hepburn Jesse Papenburg Rupeena Purewal Manish Sadarangani Laura Sauvé Karina Top Fatima Kakkar Shaun Morris
Introduction: Children with chronic neurologic and neurodevelopmental (ND) disorders are vulnerable to severe respiratory viral infection. We described comorbidity patterns among children with neurologic or ND disorders hospitalized for COVID-19, and identified neurologic diagnoses associated with severe COVID-19.
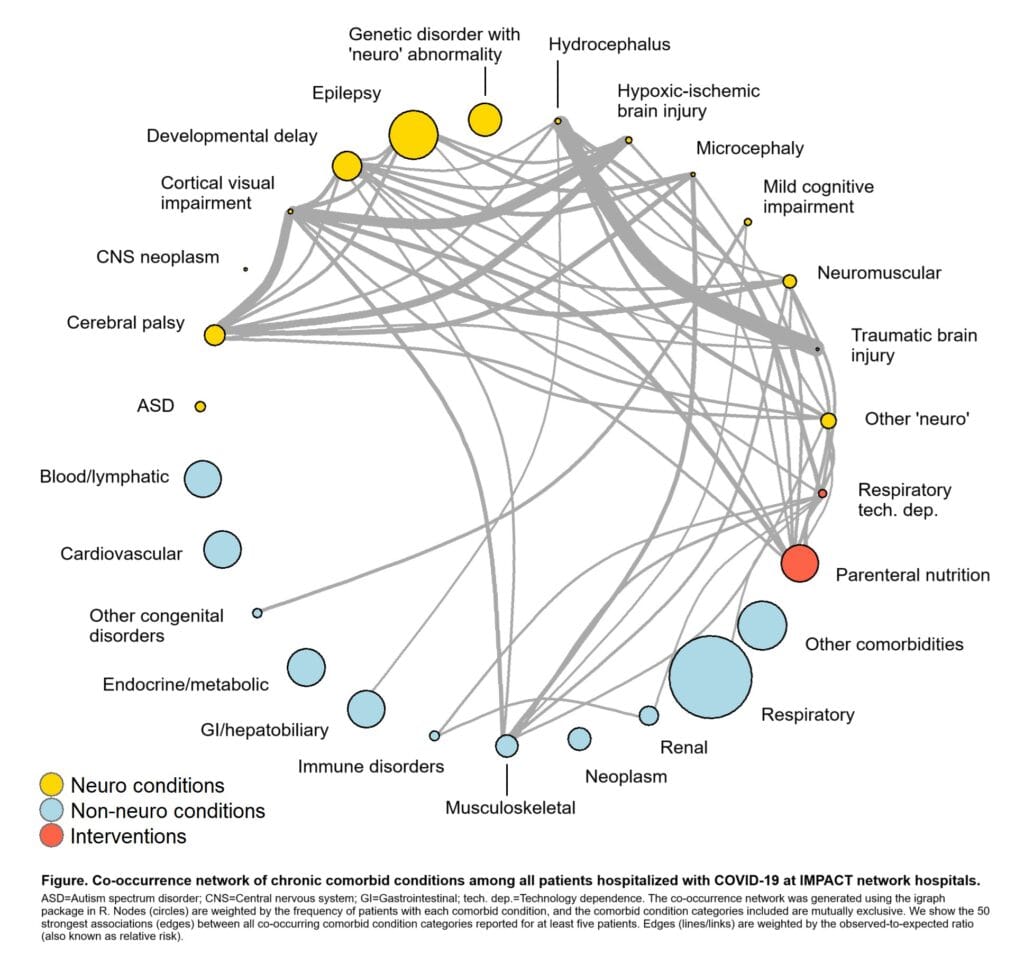
Methods: We conducted a national surveillance study at 13 paediatric hospitals in Canada, via the Canadian Paediatric Surveillance Program (April 2020–May 2021) and Canadian Immunization Monitoring Program, ACTive (June 2021–December 2022). Eligible cases were <17 years old and hospitalized for acute COVID-19. Comorbid conditions were categorized using the Medical Dictionary for Regulatory Activities. Severe COVID-19 was defined as intensive care, ventilatory, or hemodynamic support, organ system complications, or death. We conducted network analysis to describe co-occurrence of comorbid conditions, and multivariable robust Poisson regression to estimate the risk of severe COVID-19 by neurologic subgroup.
Results: Among 3218 cases hospitalized for COVID-19, 636 (19.8%) had chronic neurologic or ND disorders. Among these children, most (n=504/636) had ≥2 comorbidities with clustering between cerebral palsy, cortical visual impairment, developmental delay, epilepsy, non-neurologic musculoskeletal disorders, and/or parenteral nutrition (Figure). Most neurologic diagnoses were associated with higher risk of severe COVID-19 – epilepsy was most strongly associated (aRR 2.08, 95% CI 1.56–2.77). There was a dose response where additional neurologic diagnoses further increased risk (e.g., aRR 1.50 [95% CI 1.22–1.84] for 1 vs. 0 neurologic diagnoses; aRR 2.87 [95% CI 2.26–3.66] for ≥4 vs. 0 neurologic diagnoses).
Discussion: Children with neurologic or ND disorders frequently had multiple comorbidities. Those with neurologic multimorbidity had greatest risk of severe COVID-19, and may benefit most from immunization initiatives and early clinical intervention.