Pharmacoepidemiology
Dynamic changes in first utilization of glucagon-like peptide-1 receptor agonists, sodium-glucose cotransporter-2 inhibitors, and metabolic/bariatric surgery; an analysis of OptumLabs data, 2010-2023 Paige Wartko* Paige Wartko Rui Zhang David Arterburn Eric Johnson Jennifer F. Bobb Chixiang Chen Lisa Ross Patrick J. O’Connor Rozalina G. McCoy
Background: Diabetes and obesity are leading contributors to morbidity and mortality. Treatment options have been changing, warranting assessment of recent patterns in utilization.
Objective: To assess frequency and recent temporal patterns in utilization of glucagon-like peptide-1 receptor agonists (GLP-1RAs), sodium-glucose cotransporter-2 inhibitors (SGLT2is), and metabolic/bariatric surgery (MBS).
Study design: We used claims from OptumLabs Data Warehouse (2010–2023) for enrollees in commercial and Medicare Advantage plans with diabetes and obesity to quantify the first utilization of GLP-1RAs, SGLT2is, and MBS overall and by year.
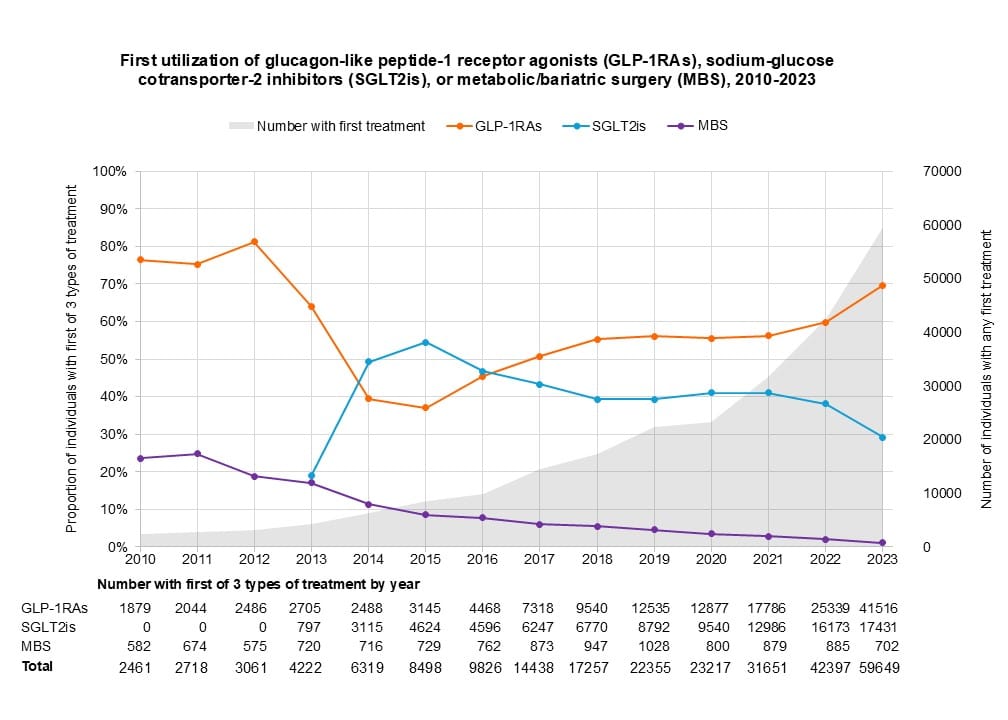
Results: We identified 248,069 individuals: 59% first used GLP-1RAs, 37% first used SGLT2is, and 4% first had MBS. Median age at first use of MBS, GLP-1RAs, and SGLT2is was 53, 60, and 63, respectively (all IQRs =17). The number of individuals using any treatment increased dramatically from 2010 to 2023 (Figure). The most common GLP-1RAs were semaglutide (41%), dulaglutide (24%), and liraglutide (16%). GLP-1RAs comprised 70% of studied treatments by 2023, with semaglutide accounting for 61% of GLP-1RA treatment. After approval in 2022, tirzepatide use increased precipitously, comprising 26% of GLP-1RA treatment by 2023. After SGLT2is’ approval in 2013, they initially surpassed GLP-1RAs; after 2016, SGLT2is comprised a lower proportion of first treatment than GLP-1RAs. The most common SGLT2is were empagliflozin (63%), dapagliflozin (20%), and canagliflozin (18%). The proportion of MBS decreased over time, although the number of individuals getting MBS did not. Sleeve gastrectomy was more common than gastric bypass after 2012.
Conclusions: We observed rapid changes over time in utilization of different, potentially more effective, and/or less burdensome, treatments for individuals with diabetes and obesity. Further studies are needed to assess the impact of these shifting patterns on health outcomes.