Neurology
Depressive symptoms and neuroimaging markers of brain aging in a racially diverse sample: a Bayesian analysis Tara E. Jenson* Tara Jenson Emma L. Gause Jingxuan Wang Sarah F. Ackley Jennifer Manly Evan Fletcher Paola Gilsanz Rachel Whitmer M. Maria Glymour Marcia Pescador Jimenez
Background: Depression has been associated with magnetic resonance imaging (MRI) measures of brain aging and atrophy in predominantly White groups, including smaller cerebral grey matter (GMV) and larger white matter hyperintensity (WMHV) volumes. It is unknown if similar associations are present, despite evidence of undertreatment of depression, in non-White groups.
Methods: A diverse sample (Asian (N=77), Black (N=290), Latino (N=90), and White (N=93)) from the Kaiser Healthy Aging and Diverse Life Experiences (age 65+) and the Study of Healthy Aging in African Americans (age 50+) based in northern California underwent MRI assessments between 2017-2022. Depressive symptoms (population average SD units) were measured at baseline using the NIH PROMIS toolbox. We used Bayesian linear regression with minimally informed priors to assess the association between depressive symptoms and log-transformed WMHV and GMV (cm3). We stratified analyses by race/ethnicity, adjusted for intracranial volume, age, gender, education, and time from baseline to MRI, and computed differences between stratum-specific estimates using a Bayesian iterative subtraction approach.
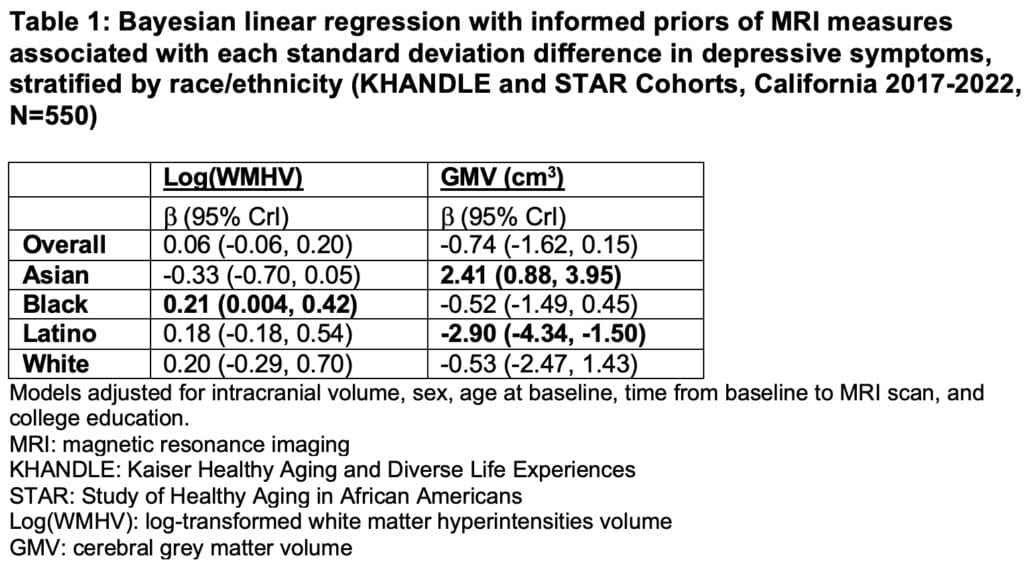
Results: Higher depressive symptoms were associated with larger log(WMHV) (0.21, 95% credible interval [CrI]: 0.004, 0.42) for Black participants; smaller GMV for Latino participants (‑2.90, 95% CrI: -4.34, -1.50), and larger GMV for Asian participants (2.41, 95% CrI: 0.88, 3.95) (Table 1). Our Bayesian iterative subtraction approach showed that per 1SD higher depressive symptoms, Asian participants had 0.54 cm3 less log(WMHV) (-0.54, 95% CrI -0.96, -0.12) and 2.95 cm3 more GMV (2.95, 95% CrI 1.14, 4.69) than Black participants (ref. group). Latino participants had 2.39 cm3 less GMV per 1 SD higher depressive symptoms than Black participants (-2.39, 95% CrI -4.07, -0.70).
Conclusion: Contrasting with prior studies using mostly White samples, we demonstrated differences in the association of depressive symptoms with MRI measures of brain aging and atrophy across racial/ethnic groups, warranting further study. A Bayesian framework may be useful to investigate understudied populations with small sample sizes, but more study is needed to determine appropriate selection of priors for understudied populations on which the literature is sparse.