Pharmacoepidemiology
Synergistic Risks: NSAIDs Use During Herpes Zoster Infection Doubles Stroke Risk – A Nationwide Case-Crossover Study Lin-Chieh Meng* Lin-Chieh Meng Hsi-Yu Lai Hui-Min Chuang Ho-Min Chen Liang-Kung Chen Fei-Yuan Hsiao
Background
Previous studies have suggested that herpes zoster (HZ) infection could trigger stroke, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs), commonly prescribed for HZ pain management, has been associated with an increased risk of stroke. However, research evaluating whether NSAID use during HZ episodes may further elevate stroke risk remains limited.
Methods
Using a population-based claims database in Taiwan (2014-2020), we identified 336,075 patients with incident stroke. A case-crossover design compared exposure to HZ and NSAIDs between the focal period (1-30 days before stroke) and the referent period (366-395 days before stroke). Conditional logistic regression estimated adjusted odds ratios (aORs) for stroke risk associated with NSAIDs use during HZ episodes. Pre-planned subgroup analyses further examined such synergistic effects on stroke subtypes, across age groups (<50, 50-64, ≥65 years) and in patients with various comorbidities, including immunocompromised and autoimmune diseases, cardiometabolic risk factors, and renal and liver diseases.
Results
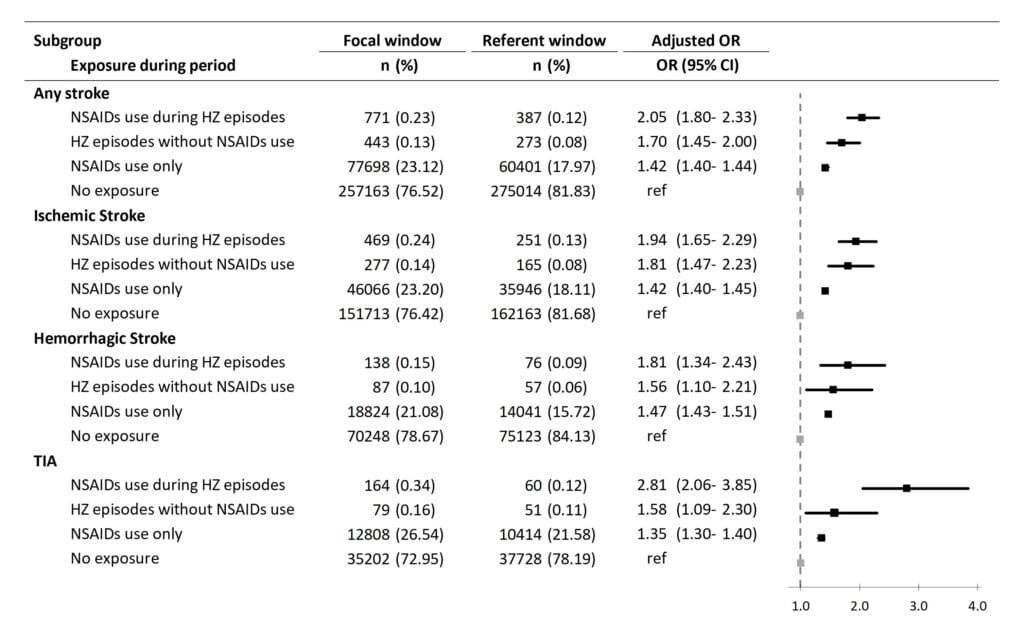
Combined HZ infection and NSAIDs use was associated with doubled stroke risk (aOR=2.05, 95% CI=1.80-2.33) compared to periods without either exposure. For specific stroke types, the adjusted ORs were 1.94 (95% CI=1.65-2.29) for ischemic stroke and 1.81 (95% CI=1.34-2.43) for hemorrhagic stroke. HZ episodes without NSAIDs (aOR=1.70, 95% CI=1.45-2.00) and NSAIDs use alone (aOR=1.42, 95% CI=1.40-1.44) showed lower but significant risk increment. In age-stratified analyses, individuals aged 65 years and older exhibited a significantly elevated stroke risk while concurrently utilizing NSAIDs during HZ episodes (aOR=2.24, 95% CI=1.92-2.62). Subgroup analyses demonstrated consistent elevated risks in patients with pre-existing comorbidities, particularly immunocompromised conditions and renal disease.
Discussion
Our findings demonstrate a significant synergistic effect between HZ infection and NSAIDs use on stroke risk, particularly among individuals aged 65 years and older or those with pre-existing cardiometabolic conditions. The optimization of pain management strategies during HZ episodes is paramount to mitigate the risk of stroke while ensuring effective management of HZ-associated pain.