Perinatal & Pediatric
Impact of increasing midwifery-led prenatal care on birth outcomes among low-risk pregnancies in a claims database: an application of the g-formula and target trial emulation Elizabeth Simmons* Elizabeth Simmons Anna Austin Mollie Wood Alyssa J. Mansfield Karen Sheffield-Abdullah Kavita Singh
Introduction: Compared to undergoing prenatal care with a physician, prenatal care with a midwife reduces risk of medical interventions and complications during labor and delivery among low-risk pregnant individuals. However, most studies that assess the relationship between midwifery-led care and birth outcomes condition on live births, potentially inducing a type of collider bias. In this study, our objective was to analyze the change in prevalence of birth outcomes under hypothetical scenarios where midwifery-led care is increased by 10%, 20% and 50% among commercially-insured, low-risk pregnant people in the United States.
Methods: We used data from the Merative MarketScan Commercial Claims and Encounters Database. Using a target trial emulation framework, we identified low-risk pregnant people aged 18-55 at delivery who initiated prenatal care in the first trimester with a viable pregnancy and with a midwife or physician. We identified outcomes (cesarean section, maternal infection, primary and secondary postpartum hemorrhage and obstetric trauma) using International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis and procedure codes. Using the nonparametric g-formula, we assessed the change in prevalence of outcomes if 10%, 20% and 50% more pregnant people enrolled in prenatal care with a midwife rather than a physician.
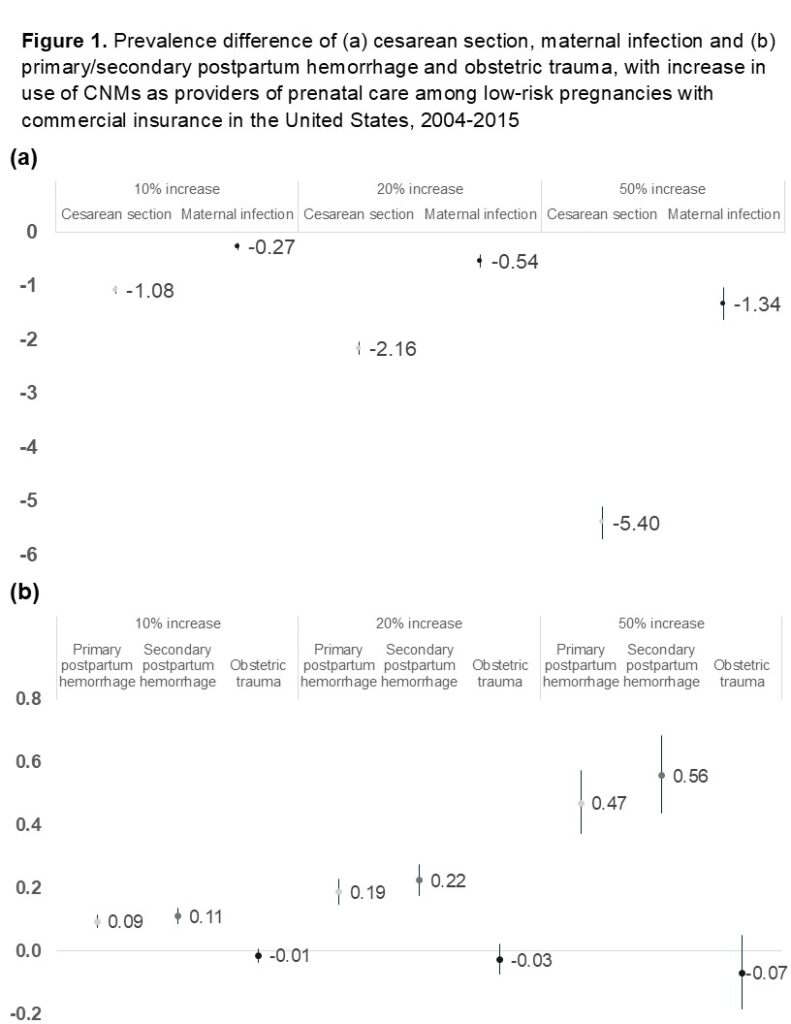
Results: With a 50% increase in the use of midwives compared with the true exposure, we found the prevalence of cesarean sections was reduced by 5.40 percentage points (95% confidence interval (CI): -5.70, -5.09) and of maternal infection decreased by 1.34 percentage points (95% CI: -1.63, -1.03), while the prevalence of primary postpartum hemorrhage increased by 0.47 percentage-points (95% CI: 0.37, 0.58) and of secondary postpartum hemorrhage of 0.56 percentage-points (95% CI: 0.44, 0.69) (Figure 1).
Conclusions: Policymakers should consider removing barriers to improve access to midwives for the US population.