COVID-19 Pandemic
Breakthrough SARS-CoV-2 Outcomes in Immune-Disordered People During the Omicron Era: A Prospective Cohort Study Fausto Andres Bustos Carrillo* Fausto Bustos Carrillo Mackenzie Zendt Viviane Callier Maureen DeGrange Anita Ginigeme Lurline Wu Bevin Manuelpillai Ana Ortega-Villa Emily E Ricotta
Background: Immune-deficient/disordered people (IDP) experience less robust immune responses to COVID-19 vaccinations than immunocompetent individuals, elevating their risk of SARS-CoV-2 infection and its adverse outcomes. Little is known about Omicron breakthrough infections in IDP. In this large prospective cohort study, we describe the rate and characteristics of Omicron breakthrough infections among IDP and healthy volunteers (HV); the occurrence of persistent infections, reinfections, post‑acute sequelae of COVID‑19 (PASC); and attitudes/behaviors regarding infection prevention.
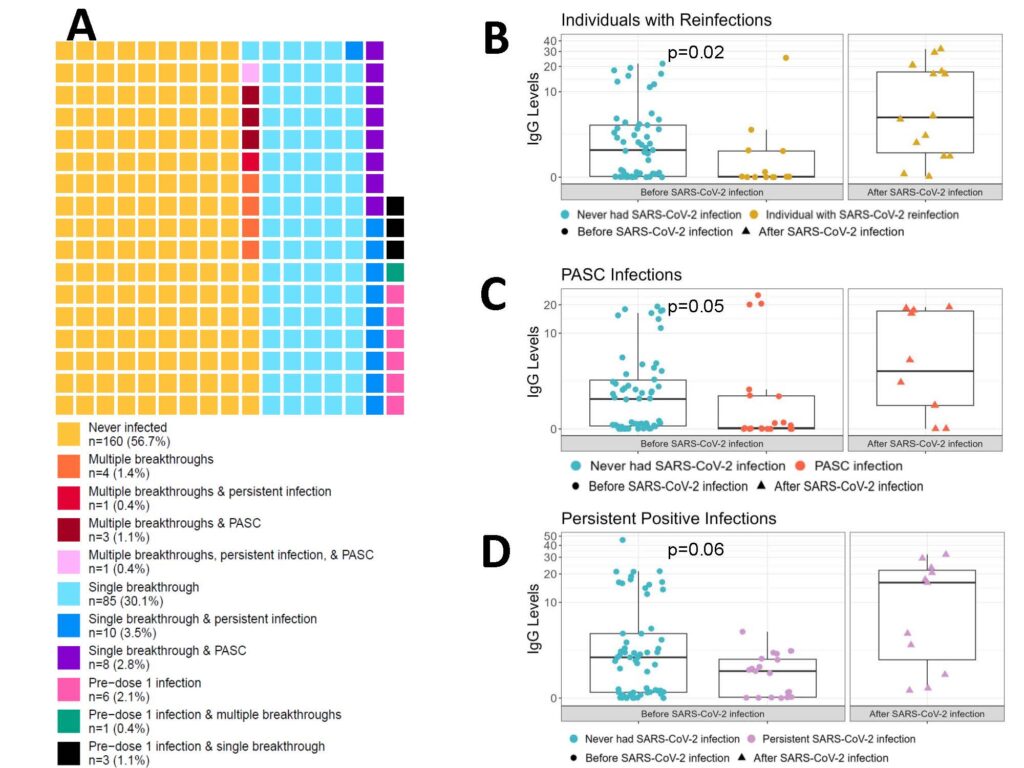
Methods: We followed 219 IDP and 63 HV throughout the US from April 2021 (peak of Alpha variant) through July 2023 (when Omicron XBB was dominant) and characterized immune responses to COVID‑19 vaccination. We quantified anti‑spike IgG titers one‑, six‑, and twelve‑months post‑vaccination and collected bi‑weekly saliva samples. Participants completed standardized surveys on COVID‑19 symptoms and preventative attitudes/behaviors.
Results: There were 88 initial breakthrough infections among IDP (incidence rate 23.7/100 person-years) and 28 among HV (27.3/100 person‑years). Incidence was 12-fold higher during than before the Omicron era. COVID‑19 symptoms were generally mild. Anti‑spike IgG titer one‑month after the most recent vaccination pre‑infection was not associated with breakthrough in either traditional analyses or an emulated trial. HV and IDP frequently practiced infection‑limiting behaviors, but IDP were more likely to continue such behaviors after vaccination. IDP experienced persistent infections, PASC, and reinfections more commonly than HV.
Conclusions: Breakthrough rates in IDP were similar to HV despite experiencing less robust immune responses to vaccination. Nevertheless, IDP experienced a slightly higher frequency of symptoms, hospitalizations, infection persistence, PASC, and reinfections than HV.