Cardiovascular
Comparison of objective coagulation parameters between clopidogrel resistant vs non-resistant patients Adriana Araceli Rodriguez Alvarez* Adriana Rodriguez Alvarez Adriana Araceli Rodriguez Alvarez Isabella Cieri Shiv Patel Mounika Boya Jang Jeongin Anahita Dua
Background: While aspirin and clopidogrel are the mainstay of therapy to prevent thrombosis post revascularization in patients with peripheral artery disease (PAD), 25% of patients are resistant to clopidogrel. Hence, identifying factors contributing to clopidogrel resistance is critical to improving patient outcome post revascularization.
Objective: To assess differences in objective coagulation parameters between clopidogrel-resistant and non-resistant patients.
Methods: Patients with PAD undergoing revascularization and taking clopidogrel between 2022 and 2024 were evaluated. Coagulation profiles were assessed using thromboelastography (TEG) on whole blood samples collected perioperatively and up to six months postoperatively. VerifyNow testing was performed at one timepoint to identify clopidogrel resistance. Patients were categorized based on their clopidogrel response: clopidogrel-resistant (>180 P2Y12 Reaction Units (PRU)) and non-resistant (<180 PRU). Descriptive statistics were calculated, and group comparisons were performed using Fisher’s exact and Wilcoxon tests.
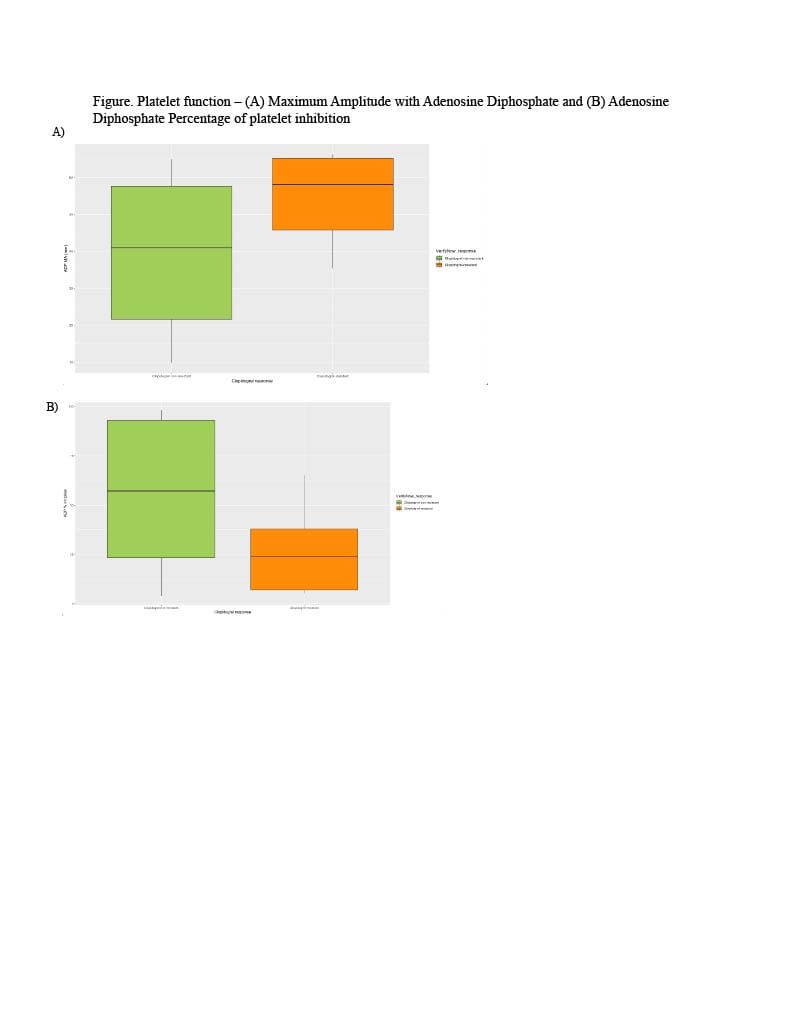
Results: A total of 53 patients were analyzed, 70% were male, and 23% were clopidogrel-resistant. Compared to the non-resistant group, the clopidogrel-resistant cohort was older, had a higher mean BMI, and exhibited higher platelet reactivity. Clopidogrel-resistant patients demonstrated faster clot formation (1.14min vs. 1.22, p<0.0001), stronger clots (54.9mm vs. 39.8, p<0.0001), and reduced clot lysis (0.97min vs. 0.69, p<0.05). These patients also showed a higher platelet aggregation (74.0% vs. 44.0%, p<0.0001) and a lower platelet inhibition (26.0% vs. 56.0%, p<0.0001), indicating a diminished response to clopidogrel and an increased risk of thrombosis.
Conclusion: Clopidogrel-resistant group exhibited faster clot formation, greater clot strength, and higher platelet aggregation. Incorporating TEG into clinical practice could help identify patients at risk of inadequate clopidogrel response.